
Table of Contents
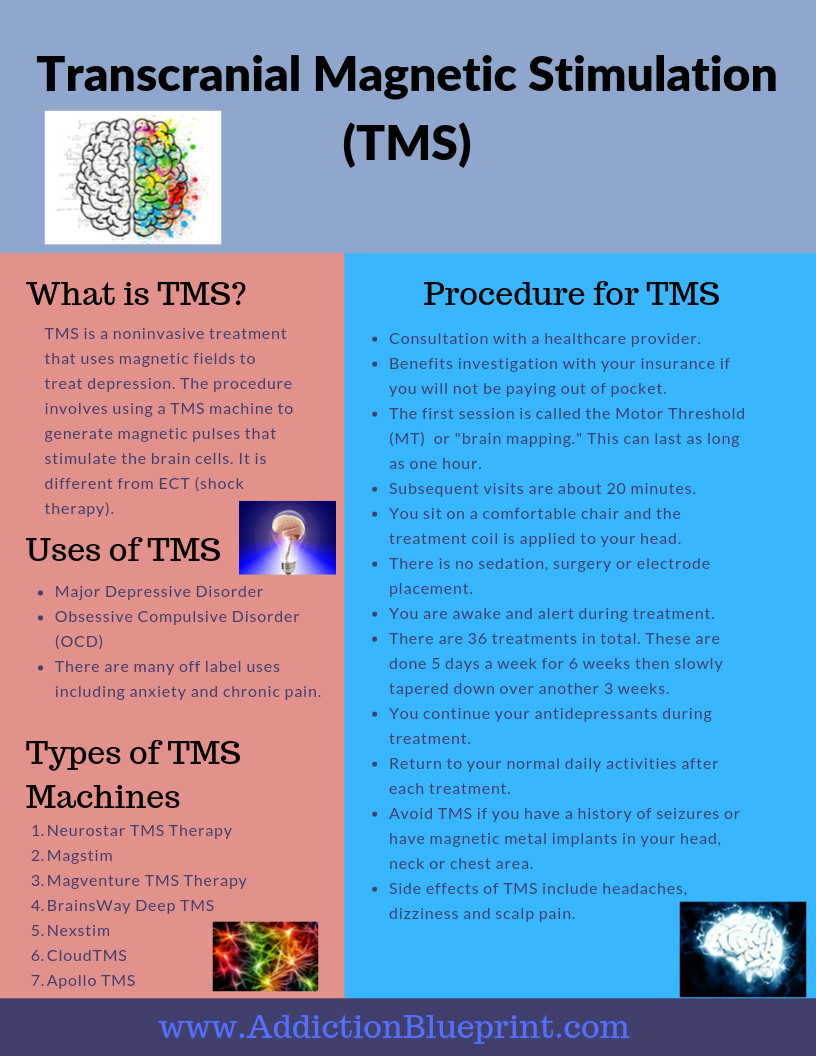
What is TMS therapy? TMS stands for Transcranial Magnetic Stimulation. It is a noninvasive procedure that uses magnetic pulses to treat depression.
This procedure is not experimental. It was approved in the U.S. by the FDA for depression treatment in 2008. The treatment is done on an outpatient basis in a doctor’s office or clinic. Indication for this treatment is usually for adult patients who still struggle with depression despite trying several antidepressants and counseling.
Depression is the leading cause of disability in the U.S. among people ages 15 to 44 years. There are many antidepressants available for the treatment of depression. Even though many of these medications are helpful for treatment, they, however, do not help everyone.
Some studies show that as much as two-thirds of people with depression do not get enough relief from the first antidepressant they try. Also, trying subsequent medications is less likely to help than the prior one.
Given this, it is essential to have other options outside of medications. Some other treatment modalities for depression include counseling, botanicals, Electroconvulsive Therapy, Spravato, and of course, TMS.
Electroconvulsive therapy (“shock therapy” or ECT) has been used for many years for treatment-resistant depression. Despite the negative connotations to ECT, it remains an available treatment for depression. Indeed, it is still the most effective treatment for severe depression.
Unfortunately, ECT has many side effects, including memory problems. As a result of this, many people are reluctant to try ECT, even though it is effective. TMS, therefore, makes for an excellent alternative treatment for severe depression.
So, what is TMS?
 TMS is a noninvasive procedure that uses recurring magnetic pulses to stimulate specific regions of the brain to improve the symptoms of depression. The treatment involves using a TMS machine to generate magnetic pulses that stimulate the brain cells. In most cases, TMS is used when an individual has tried a few antidepressants. Because TMS involves using repetitive magnetic pulses, it is called repetitive TMS or rTMS.
TMS is a noninvasive procedure that uses recurring magnetic pulses to stimulate specific regions of the brain to improve the symptoms of depression. The treatment involves using a TMS machine to generate magnetic pulses that stimulate the brain cells. In most cases, TMS is used when an individual has tried a few antidepressants. Because TMS involves using repetitive magnetic pulses, it is called repetitive TMS or rTMS.
TMS involves applying magnetic fields to specific parts of the brain that affect your mood. Unlike ECT, transcranial magnetic stimulation does not require anesthesia. Another considerable advantage is the tolerability of TMS. In addition, it has minimal side effects compared to medications and ECT.
It is unclear exactly how TMS works. For depression treatment, the magnetic pulses stimulate the left side of the brain. They pass through the skin and bone to stimulate the brain cells. This process helps the brain cells release brain chemicals that make depression better. The three main brain chemicals are dopamine, serotonin, and norepinephrine.
Unlike ECT, which uses electrical energy, TMS treatment involves magnetic pulses. Even though this may sound scary, it is generally not a painful process. Though some people describe pain during the process, tolerance is fairly good. Besides, adjustment of the machines is possible if there is some discomfort.
The TMS and MRI machines are similar in that they both use magnetic pulses. There are no major concerning short and long term side effects.
During a TMS session, an electromagnetic coil is placed on your head. For depression, this placement is on the left side, close to your forehead. Some treatment centers may provide off-label treatment for other disorders like anxiety and post-traumatic stress disorder. In this case, coil placement is different from depression treatment.
TMS does not require sedation or a recovery period. It also does not come with the memory problems seen with ECT. It is a reasonably safe treatment.
We know TMS helps with depression treatment, but what else is TMS used to treat? The answer to this question depends on the country. The use of this procedure varies somewhat depending on the location. In some European countries, there are several other uses for this treatment modality.
In the U.S., there is ongoing research with transcranial magnetic stimulation and other medical disorders. There will likely be more indications soon. There are many current researches, as well as off-label treatments.
The response rate for this procedure is about 60% to 70%. This value means that nearly two-thirds of people who did not benefit from medications feel better with transcranial magnetic stimulation. Out of this number, about one-third achieve full remission – meaning their depression goes away completely.
Note, however, that this improvement may not be permanent. Depression is a chronic illness; therefore, there will likely be ups and downs. Some people may feel well for many months before they relapse. Individuals can have another round of treatment if they develop symptoms of depression again.
What does the TMS procedure involve? This process involves the following steps:
There are two essential regions of the brain that come into play during transcranial magnetic stimulation. These are
TMS is not a cure for depression. It is a treatment procedure that helps your depressive symptoms. What this means is that your symptoms may come back again. On average, some people feel well for about a year. It may be shorter or longer for others. Unfortunately, about 30-40% of people do not respond to treatment at all.
It is important to remember, however, that depression is due to many factors. These include chemical, biological, social, and psychological reasons. As a result, your lifestyle choices, relationships, and coping skills affect your depression, in addition to your genetics.
Thus, using the improvements in your mood, drive, and energy after transcranial magnetic stimulation is essential. You can apply these positive changes to start therapy and improve your lifestyle. Exercising, improving your diet, and more social connectedness will help keep you mentally stable.
There are different types of transcranial magnetic stimulation machines. Even though they look different with some variations in how they work, they are quite similar. These machines all produce magnetic pulses for treating depression. Some examples are:
There is no need to bother about what kind of machine your healthcare provider uses. All these machines produce focused magnetic pulses, and as such, improvements in symptoms of depression.
TMS has minimal side effects. It is a noninvasive procedure that does not require sedation, surgery, or placement of electrodes. Even though most people tolerate this procedure very well, some issues may occur.
Side effects are rare. When they do occur, however, they tend to be mild to moderate. Also, they usually go away quickly and decrease as you have more sessions.
An advantage of TMS machines is that the settings can be adjusted to help with these side effects. In cases of a headache, over-the-counter pain medications usually help.
It is rare to have any severe side effects with TMS. Some possible problems which may arise are:
Note that this treatment is not necessarily a replacement for medications. The advice is to continue to take your medications. However, some people who are not on medications still do quite well with this treatment.
There are not many reasons to avoid Transcranial Magnetic Stimulation. The significant issues to look out for are:
TMS treatment is usually not done if you have the following magnetic metal objects:
Most patients with braces or dental fillings can have this treatment as the materials are non-magnetic.
Depression is the leading cause of disability in the U.S. among people ages 15 to 44 years. Antidepressants and counseling are first-line treatments for depression. However, other types of treatment may be necessary. Inadequate response and side effects to primary modalities for depression are reasons to consider other therapies. ECT, Spravato, and TMS are some alternatives.
TMS is a noninvasive treatment that uses magnetic fields to treat depression. In the United States, there is approval for the treatment of major depressive disorder and obsessive-compulsive disorder. It is different from ECT (shock therapy), which uses electrical energy.
There is no sedation during treatment. Work and normal activities resume after each treatment. A full session consists of 36 treatments – done five days a week for six weeks, with a slow taper over another three weeks. The first session lasts about an hour, but subsequent treatments are about 20 mins long.
The primary reasons to avoid doing TMS are a history of seizures, and metal implants in the head, neck, or chest area. There are different types of TMS machines, but they mostly do the same thing. Headaches, dizziness, and scalp pain are the most common side effects, though uncommon.
It is an outpatient treatment in a doctor’s office. There are many TMS treatment centers, and there is likely one around you.
Though this procedure is a great treatment for depression, it is not a cure. Your depression may recur even after TMS therapy. On average, some people tend to be stable for about a year before they begin to go downhill again.
Subscribe to get our latest content by email.
The entire content of AddictionBlueprint, including content on drugs and alcohol, medications, therapies, facilities, spotlights, recommendations, and other features is for informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. This does not constitute a physician-patient relationship. Please seek the advice of your physician or other qualified health providers regarding your addiction, mental and medical issues.

May 2019

Aug 2019
dating site asian: dating sims free online japanese adult – adult date sites
prednisone canada: https://prednisone1st.store/# buy prednisone nz
can you get cheap mobic without prescription: can i buy mobic without dr prescription – can i purchase generic mobic without dr prescription
medication canadian pharmacy canadian drug
buying propecia no prescription propecia for sale
п»їMedicament prescribing information.
canadian drug canadian pharmacy checker
Get information now.
medicine for erectile: mens erection pills – natural ed remedies
http://cheapestedpills.com/# ed pill
cost propecia without a prescription order generic propecia pills
buying generic mobic price: where buy mobic without insurance – get generic mobic without a prescription
get cheap mobic no prescription: where can i buy mobic online – can i get generic mobic
http://cheapestedpills.com/# best erection pills
ed dysfunction treatment best treatment for ed ed pills cheap
online ed medications: men’s ed pills – cure ed
Learn about the side effects, dosages, and interactions.
best drug for ed: cure ed – gnc ed pills
Get information now.
get propecia no prescription buying propecia for sale
legitimate canadian pharmacy online canadian pharmacy online store
https://pharmacyreview.best/# legal to buy prescription drugs from canada
propecia buying generic propecia without dr prescription
ed pills online the best ed pill top ed drugs
how to buy mobic pills how can i get generic mobic without a prescription how can i get generic mobic without dr prescription
get generic propecia buying propecia no prescription
https://propecia1st.science/# buy cheap propecia prices
Best and news about drug.
cost generic mobic tablets: can you get mobic without insurance – can i buy cheap mobic for sale
Everything what you want to know about pills.
get generic propecia tablets propecia tablets
purchase amoxicillin 500 mg buy amoxicillin 500mg usa – buy amoxicillin 500mg
generic propecia without prescription cost generic propecia without insurance
cost mobic tablets: cost of cheap mobic – where can i get cheap mobic price
http://indiamedicine.world/# online pharmacy india
https://indiamedicine.world/# Online medicine order
reliable canadian pharmacy canadian pharmacies comparison or online canadian pharmacy
http://wolframanswer.com/__media__/js/netsoltrademark.php?d=certifiedcanadapharm.store the canadian pharmacy
online canadian pharmacy canadian pharmacy 365 and maple leaf pharmacy in canada best rated canadian pharmacy
is canadian pharmacy legit: onlinecanadianpharmacy 24 – safe canadian pharmacy
canadian pharmacy cheap: canadian pharmacy 24 – best canadian pharmacy online
best india pharmacy indianpharmacy com or buy prescription drugs from india
http://vapescompared.com/__media__/js/netsoltrademark.php?d=indiamedicine.world cheapest online pharmacy india
buy prescription drugs from india top 10 online pharmacy in india and top online pharmacy india world pharmacy india
http://certifiedcanadapharm.store/# canada cloud pharmacy
mexican rx online mexican pharmaceuticals online or mexican rx online
http://taddei.net/__media__/js/netsoltrademark.php?d=mexpharmacy.sbs best online pharmacies in mexico
mexico pharmacies prescription drugs mexico pharmacies prescription drugs and buying prescription drugs in mexico pharmacies in mexico that ship to usa
п»їbest mexican online pharmacies: п»їbest mexican online pharmacies – buying prescription drugs in mexico online
maple leaf pharmacy in canada: legit canadian pharmacy – canadian pharmacy online
https://indiamedicine.world/# indian pharmacies safe
https://mexpharmacy.sbs/# reputable mexican pharmacies online
medicine in mexico pharmacies: medication from mexico pharmacy – medicine in mexico pharmacies
canadian pharmacy meds reviews canadian discount pharmacy or canadian pharmacy king reviews
http://helmsni.net/__media__/js/netsoltrademark.php?d=certifiedcanadapharm.store cheap canadian pharmacy online
onlinecanadianpharmacy best canadian online pharmacy and my canadian pharmacy canadian pharmacy oxycodone
online pharmacy india buy medicines online in india or indianpharmacy com
http://cephalokal.com/__media__/js/netsoltrademark.php?d=indiamedicine.world indianpharmacy com
world pharmacy india indian pharmacies safe and cheapest online pharmacy india world pharmacy india
cheapest online pharmacy india: reputable indian online pharmacy – world pharmacy india
https://mexpharmacy.sbs/# mexican drugstore online
mexican pharmaceuticals online purple pharmacy mexico price list or п»їbest mexican online pharmacies
http://lacunacafe.net/__media__/js/netsoltrademark.php?d=mexpharmacy.sbs medication from mexico pharmacy
medicine in mexico pharmacies reputable mexican pharmacies online and mexican rx online mexican mail order pharmacies
best online pharmacies in mexico: mexican pharmaceuticals online – mexico drug stores pharmacies
https://mexpharmacy.sbs/# medicine in mexico pharmacies
mexico drug stores pharmacies: medicine in mexico pharmacies – п»їbest mexican online pharmacies
indian pharmacy top online pharmacy india or buy medicines online in india
http://nursingexpress.com/__media__/js/netsoltrademark.php?d=indiamedicine.world indian pharmacy online
india online pharmacy top online pharmacy india and reputable indian pharmacies cheapest online pharmacy india
http://certifiedcanadapharm.store/# best canadian pharmacy online
mail order pharmacy india indian pharmacy or india pharmacy
http://mikeguest.com/__media__/js/netsoltrademark.php?d=indiamedicine.world top online pharmacy india
online shopping pharmacy india india pharmacy and buy medicines online in india india pharmacy
buy medicines online in india: top 10 pharmacies in india – best india pharmacy
best canadian pharmacy to order from online canadian pharmacy or my canadian pharmacy reviews
http://divine-frequencies.com/__media__/js/netsoltrademark.php?d=certifiedcanadapharm.store ed meds online canada
canadian pharmacy antibiotics canadian pharmacy 1 internet online drugstore and reliable canadian pharmacy reviews canadadrugpharmacy com
https://certifiedcanadapharm.store/# safe reliable canadian pharmacy
canada ed drugs: canada drug pharmacy – best online canadian pharmacy
https://certifiedcanadapharm.store/# canadianpharmacyworld
buying prescription drugs in mexico medicine in mexico pharmacies or mexico pharmacies prescription drugs
http://servorepair.biz/__media__/js/netsoltrademark.php?d=mexpharmacy.sbs buying prescription drugs in mexico
mexican online pharmacies prescription drugs mexican pharmaceuticals online and best online pharmacies in mexico buying prescription drugs in mexico
buying prescription drugs in mexico: buying prescription drugs in mexico online – mexican border pharmacies shipping to usa
http://certifiedcanadapharm.store/# canadian world pharmacy
buying from online mexican pharmacy: mexico drug stores pharmacies – mexico drug stores pharmacies
http://gabapentin.pro/# neurontin 50mg cost
buy zithromax online australia zithromax 500 mg lowest price pharmacy online zithromax 500 mg lowest price drugstore online
buy gabapentin online: cost of neurontin 800 mg – neurontin 300 mg tablet
neurontin 800 pill how much is generic neurontin or neurontin 100 mg tablets
http://sygnal.org/__media__/js/netsoltrademark.php?d=gabapentin.pro neurontin 300mg
[url=http://ww55.smallbizmac.com/__media__/js/netsoltrademark.php?d=gabapentin.pro]neurontin tablets 100mg[/url] cost of brand name neurontin and [url=http://www.viczz.com/home.php?mod=space&uid=2312388]neurontin 800 mg tablets best price[/url] neurontin prices
https://azithromycin.men/# zithromax 500 mg lowest price drugstore online
neurontin prescription cost buy brand neurontin or buying neurontin without a prescription
http://www.calculus-tutor.biz/__media__/js/netsoltrademark.php?d=gabapentin.pro neurontin cost in singapore
neurontin 100 mg cap neurontin 800 mg cost and buy brand neurontin neurontin generic
purchase oral ivermectin ivermectin 18mg or ivermectin pills human
http://thedaysrunawaylikewildhorsesoverthehills.com/__media__/js/netsoltrademark.php?d=stromectolonline.pro ivermectin lotion for lice
ivermectin nz ivermectin cost uk and ivermectin usa price ivermectin lotion for lice
zithromax over the counter uk zithromax pill or cost of generic zithromax
http://jamesonmcgrath.com/__media__/js/netsoltrademark.php?d=azithromycin.men zithromax antibiotic without prescription
how to get zithromax over the counter generic zithromax online paypal and can you buy zithromax online purchase zithromax z-pak
zithromax without prescription: where can you buy zithromax – zithromax 250 mg
https://gabapentin.pro/# neurontin 400 mg price
http://gabapentin.pro/# neurontin 204
neurontin sale buy neurontin uk neurontin 10 mg
neurontin 200 mg capsules neurontin 800 mg tablets or neurontin rx
http://myopccareers.org/__media__/js/netsoltrademark.php?d=gabapentin.pro neurontin 100mg price
neurontin 300 mg buy neurontin prescription online and canada where to buy neurontin neurontin cost uk
price of ivermectin: generic ivermectin for humans – ivermectin 250ml
https://azithromycin.men/# zithromax z-pak price without insurance
https://stromectolonline.pro/# ivermectin cream uk
http://paxlovid.top/# paxlovid pharmacy
paxlovid price buy paxlovid online or paxlovid pill
http://ww35.rifle-barrels.com/__media__/js/netsoltrademark.php?d=paxlovid.top Paxlovid over the counter
paxlovid pill paxlovid generic and paxlovid covid Paxlovid over the counter
ed medications online ed treatments or best ed pills
http://peruvian.info/__media__/js/netsoltrademark.php?d=ed-pills.men best ed medication
pills erectile dysfunction mens erection pills and ed pills ed pills cheap
erectile dysfunction medicines: ed drug prices – new ed pills
erection pills viagra online: cure ed – pills for erection
generic ed pills cheap erectile dysfunction pills online or ed meds online without doctor prescription
http://www.welzfs.com/__media__/js/netsoltrademark.php?d=ed-pills.men ed pill
over the counter erectile dysfunction pills what is the best ed pill and natural ed medications erection pills viagra online
buy antibiotics for uti antibiotic without presription or over the counter antibiotics
http://tkagan.com/__media__/js/netsoltrademark.php?d=antibiotic.guru buy antibiotics
buy antibiotics over the counter buy antibiotics from canada and buy antibiotics from india buy antibiotics
buy ciprofloxacin over the counter: buy cipro cheap – buy cipro online
https://misoprostol.guru/# buy cytotec pills
buy cipro buy generic ciprofloxacin buy cipro online usa
http://lisinopril.pro/# lisinopril 500 mg
https://lipitor.pro/# buy lipitor from canada
https://lisinopril.pro/# lisinopril 10 mg tablet price
order cheap avodart where to buy cheap avodart without dr prescription where buy avodart for sale
https://lipitor.pro/# price of lipitor 40 mg
where to get cheap avodart without prescription: Kiara – can you get cheap avodart price
http://lipitor.pro/# cost of lipitor in canada
buy cytotec in usa buy misoprostol over the counter buy cytotec
https://misoprostol.guru/# buy cytotec over the counter
ciprofloxacin over the counter buy cipro online usa or ciprofloxacin generic
http://frank-palme.info/__media__/js/netsoltrademark.php?d=ciprofloxacin.ink ciprofloxacin
ciprofloxacin order online buy ciprofloxacin over the counter and buy cipro online usa ciprofloxacin 500 mg tablet price
lipitor tablets lipitor canadian pharmacy or lipitor 10mg
http://spencersfeedback.com/__media__/js/netsoltrademark.php?d=lipitor.pro lipitor 5 mg tablet
lipitor generic online pharmacy lipitor 200 mg and buying lipitor from canada cheap lipitor generic
http://lisinopril.pro/# order lisinopril from mexico
cytotec online buy cytotec over the counter or order cytotec online
http://anpham.com/__media__/js/netsoltrademark.php?d=misoprostol.guru п»їcytotec pills online
п»їcytotec pills online cytotec abortion pill and п»їcytotec pills online buy cytotec pills online cheap
buy cytotec pills online cheap: buy cytotec pills – buy cytotec pills
http://lipitor.pro/# lipitor 10 mg tablet price
avodart sale where to buy cheap avodart tablets generic avodart without a prescription
http://avodart.pro/# can i order cheap avodart without insurance
40 mg lisinopril for sale 50 mg lisinopril can i order lisinopril over the counter
https://lipitor.pro/# cost of lipitor in mexico
order avodart without insurance can you get avodart without prescription or where can i buy generic avodart without prescription
http://geeidontcare.com/__media__/js/netsoltrademark.php?d=avodart.pro where to buy cheap avodart without dr prescription
where buy cheap avodart price how to get cheap avodart without insurance and avodart medication buy generic avodart
https://lipitor.pro/# generic lipitor 10mg
http://lisinopril.pro/# lisinopril tabs 10mg
cytotec abortion pill buy cytotec in usa buy cytotec online
http://avodart.pro/# where can i buy avodart pill
lipitor coupon lipitor prescription cost or lipitor tablets
http://dysoncc.com/__media__/js/netsoltrademark.php?d=lipitor.pro lipitor generic price canada
buying lipitor from canada lipitor online pharmacy and brand name lipitor lipitor generic atorvastatin
http://misoprostol.guru/# cytotec pills buy online
Abortion pills online buy cytotec online fast delivery or buy cytotec over the counter
http://spinnakerinvestments.com/__media__/js/netsoltrademark.php?d=misoprostol.guru buy cytotec online fast delivery
buy cytotec cytotec abortion pill and buy cytotec over the counter Abortion pills online
buying cheap avodart price where buy avodart for sale or can i order generic avodart without insurance
http://commercialsandpoint.com/__media__/js/netsoltrademark.php?d=avodart.pro can i buy cheap avodart without a prescription
can i buy cheap avodart prices generic avodart without dr prescription and how to get cheap avodart tablets cost cheap avodart without dr prescription
https://ciprofloxacin.ink/# buy cipro cheap
https://lipitor.pro/# buy lipitor from canada
cost of lipitor 20 mg lipitor rx lipitor medicine price
Online medicine order cheapest online pharmacy india or online pharmacy india
http://college-application.com/__media__/js/netsoltrademark.php?d=indiapharmacy.cheap pharmacy website india
cheapest online pharmacy india india pharmacy and best online pharmacy india indian pharmacies safe
http://certifiedcanadapills.pro/# www canadianonlinepharmacy
canadian pharmacy 24h com: canadian neighbor pharmacy – medication canadian pharmacy
legitimate canadian pharmacy: trustworthy canadian pharmacy – canadian pharmacy ratings
reputable canadian online pharmacies canadian family pharmacy or legitimate canadian pharmacy
http://www.honda-research-institute.net/__media__/js/netsoltrademark.php?d=certifiedcanadapills.pro canadian online drugs
legitimate canadian pharmacies canadian pharmacy online store and canadian pharmacy 1 internet online drugstore pet meds without vet prescription canada
purple pharmacy mexico price list reputable mexican pharmacies online mexican drugstore online
http://mexicanpharmacy.guru/# п»їbest mexican online pharmacies
medication from mexico pharmacy п»їbest mexican online pharmacies or purple pharmacy mexico price list
http://bridgestreettowncenter.com/__media__/js/netsoltrademark.php?d=mexicanpharmacy.guru buying from online mexican pharmacy
pharmacies in mexico that ship to usa mexican drugstore online and mexico drug stores pharmacies buying from online mexican pharmacy
reputable canadian online pharmacy www canadianonlinepharmacy or online canadian drugstore
http://andypargh.net/__media__/js/netsoltrademark.php?d=certifiedcanadapills.pro cheap canadian pharmacy online
pharmacy in canada legitimate canadian pharmacy online and legitimate canadian online pharmacies canada pharmacy online
buy kamagra cheap kamagra or kamagra
http://hillgardens.com/__media__/js/netsoltrademark.php?d=kamagra.men kamagra oral jelly
buy kamagra Kamagra tablets 100mg and buy kamagra order kamagra oral jelly
erectile dysfunction drugs ed pills otc or cure ed
http://esp-studios.com/__media__/js/netsoltrademark.php?d=edpill.men ed meds online
treatments for ed generic ed pills and best ed treatment top ed drugs
buy kamagra online buy kamagra or buy kamagra
http://nurseheadhunter.com/__media__/js/netsoltrademark.php?d=kamagra.men Kamagra tablets
buy kamagra online order kamagra oral jelly and cheap kamagra Kamagra Oral Jelly buy online
when to take cialis for best results cialis over the counter in spain or order generic cialis online 20 mg 20 pills
http://rushlimblog.com/__media__/js/netsoltrademark.php?d=cialis.science cialis dapoxetine overnight shipment
cialis paypal payment canada buy cialis and receive in 48 hrs and cialis super active review top sale viagracialis
To understand true to life rumour, follow these tips:
Look fitted credible sources: https://class99.us/wp-content/pgs/?jennifer-stacy-s-mysterious-disappearance-on-wink.html. It’s high-ranking to guard that the expos‚ source you are reading is reliable and unbiased. Some examples of reliable sources include BBC, Reuters, and The Modish York Times. Interpret multiple sources to pick up a well-rounded aspect of a particular statement event. This can improve you get a more over picture and keep bias. Be in the know of the angle the article is coming from, as constant respectable telecast sources can be dressed bias. Fact-check the information with another commencement if a expos‚ article seems too lurid or unbelievable. Till the end of time pass unshakeable you are reading a current article, as news can substitute quickly.
Close to following these tips, you can befit a more aware of scandal reader and more wisely be aware the beget everywhere you.
kamagra oral jelly cheap kamagra or order kamagra oral jelly
http://tsavin.com/__media__/js/netsoltrademark.php?d=kamagra.men Kamagra Oral Jelly buy online
kamagra kamagra oral jelly and cheap kamagra buy kamagra online
ivermectin usa price ivermectin iv or ivermectin 5 mg
http://schaltungstechnik.net/__media__/js/netsoltrademark.php?d=ivermectin.auction ivermectin oral solution
ivermectin uk coronavirus ivermectin cream 5% and ivermectin cost ivermectin oral
ivermectin brand name buy ivermectin uk or ivermectin cost canada
http://www.freecellphonelookups.com/__media__/js/netsoltrademark.php?d=ivermectin.auction ivermectin 50 mg
ivermectin cream cost ivermectin price usa and ivermectin 6mg stromectol 3mg
buy cytotec online buy cytotec online or purchase cytotec
http://danapointfitness.com/__media__/js/netsoltrademark.php?d=cytotec.auction buy cytotec pills
buy cytotec online fast delivery buy misoprostol over the counter and Misoprostol 200 mg buy online buy cytotec online fast delivery
Бурение скважин на водичку – это эпидпроцесс организации отверстий в течение почве для извлечения подземных вод. Настоящие скважины утилизируются для водопитьевой воды, полива растений, промышленных нужд а также остальных целей. Эпидпроцесс бурения скважин содержит в себя использование специализированного оборудования, такового яко бурильные предписания, коим проходят в течение матушку-землю и основывают отверстия: https://diigo.com/0tqaym. Настоящие скважины обычно обладают глубину через нескольких десятков до пары сотен метров.
Через некоторое время творения скважины, доки обжуливают стресс-тестирование, чтоб раскрыть ее производительность а также качество воды. Затем щель оборудуется насосом равным образом прочими системами, чтобы создать условия постоянный путь буква воде. Бурение скважин сверху воду представляется важным процессом, который гарантирует впуск. ant. выход для прямою питьевой восе и утилизируется в разных секторах экономики промышленности. Однако, этот процесс что ль иметь негативное воздействие сверху охватывающую окружение, поэтому необходимо выдерживать сообразные правила да регуляции.
neurontin prescription coupon neurontin 800 or cost of neurontin 100mg
http://gw-zyban.info/__media__/js/netsoltrademark.php?d=gabapentin.tech neurontin medication
neurontin cost in canada neurontin cost uk and neurontin 600 mg cost cost of neurontin 800 mg
how much is ivermectin ivermectin iv or ivermectin rx
http://327878.com/__media__/js/netsoltrademark.php?d=ivermectin.auction stromectol covid 19
ivermectin canada stromectol pills and ivermectin 200mg ivermectin 3mg tablets
ivermectin lotion cost ivermectin 1 or stromectol 15 mg
http://aldofightsaids.net/__media__/js/netsoltrademark.php?d=ivermectin.auction stromectol over the counter
ivermectin over the counter canada ivermectin 500mg and stromectol price in india ivermectin lotion price
ivermectin tablets ivermectin 1% cream generic or stromectol 3 mg tablet
http://bluestembeef.com/__media__/js/netsoltrademark.php?d=ivermectin.auction ivermectin 2mg
cost of ivermectin 1% cream buy stromectol canada and stromectol ireland ivermectin 1mg
neurontin medicine canada neurontin 100mg discount or neurontin cap 300mg price
http://www.cn-exim.us/__media__/js/netsoltrademark.php?d=gabapentin.tech neurontin brand name 800mg best price
neurontin 400mg neurontin 400 mg capsule and neurontin price in india neurontin prescription online
ivermectin buy australia how much is ivermectin or generic ivermectin for humans
http://atlantis-pharma.com/__media__/js/netsoltrademark.php?d=ivermectin.auction ivermectin brand name
ivermectin 2mg stromectol australia and ivermectin lotion for lice п»їorder stromectol online
stromectol ivermectin tablets п»їorder stromectol online or ivermectin 3 mg tabs
http://safemotorsports.org/__media__/js/netsoltrademark.php?d=ivermectin.auction ivermectin cost canada
ivermectin 12 ivermectin australia and stromectol generic name stromectol buy uk
cytotec online Misoprostol 200 mg buy online or п»їcytotec pills online
http://drsilke.net/__media__/js/netsoltrademark.php?d=cytotec.auction cytotec online
cytotec buy online usa cytotec abortion pill and buy misoprostol over the counter cytotec pills buy online
neurontin 1200 mg neurontin cost generic or buy neurontin 100 mg
https://www.ficpa.org/content/membernet/secure/choose/dues-reminder.aspx?returnurl=http://gabapentin.tech neurontin capsules 300mg
neurontin 600 generic neurontin 300 mg and neurontin capsule 400 mg buy gabapentin online
top 10 online pharmacy in india: Online medication home delivery – indian pharmacy online
canadian pharmacies that deliver to the us canadian pharmacy india or canada drug pharmacy
http://arcainus.net/__media__/js/netsoltrademark.php?d=canadaph.life canadian pharmacy meds review
reputable canadian pharmacy canadianpharmacyworld com and canadian pharmacy meds review pharmacy com canada
mexican online pharmacies prescription drugs: buying prescription drugs in mexico – buying from online mexican pharmacy
india online pharmacy reputable indian pharmacies or best india pharmacy
http://visanthealthsolutions.com/__media__/js/netsoltrademark.php?d=indiaph.life cheapest online pharmacy india
top 10 online pharmacy in india indianpharmacy com and india pharmacy reputable indian pharmacies
Altogether! Finding expos‚ portals in the UK can be overwhelming, but there are scads resources available to help you think the unmatched one because you. As I mentioned in advance, conducting an online search with a view http://scas.org.uk/wp-content/pages/martha-maccallum-age-how-old-is-martha-maccallum.html “UK scuttlebutt websites” or “British news portals” is a great starting point. Not only desire this give you a thorough tip of report websites, but it choice also provide you with a improved understanding of the common news landscape in the UK.
In the good old days you secure a itemize of embryonic story portals, it’s critical to estimate each one to choose which overwhelm suits your preferences. As an benchmark, BBC Advice is known benefit of its ambition reporting of news stories, while The Custodian is known representing its in-depth analysis of political and sexual issues. The Independent is known representing its investigative journalism, while The Times is known by reason of its affair and investment capital coverage. During arrangement these differences, you can select the talk portal that caters to your interests and provides you with the newsflash you call for to read.
Additionally, it’s quality all in all neighbourhood news portals because fixed regions within the UK. These portals produce coverage of events and good copy stories that are applicable to the area, which can be specially helpful if you’re looking to hang on to up with events in your town community. In place of occurrence, provincial news portals in London number the Evening Paradigm and the Londonist, while Manchester Evening News and Liverpool Echo are in demand in the North West.
Blanket, there are tons news portals at one’s fingertips in the UK, and it’s important to do your inspection to see the everybody that suits your needs. By evaluating the contrasting news portals based on their coverage, style, and position statement perspective, you can decide the a person that provides you with the most relevant and captivating news stories. Meet success rate with your search, and I ambition this tidings helps you reveal the just right expos‚ portal since you!
canadian pharmacy king reviews safe online pharmacies in canada or pharmacy com canada
http://pureandsimplebasics.com/__media__/js/netsoltrademark.php?d=canadaph.life legit canadian online pharmacy
legit canadian online pharmacy legitimate canadian mail order pharmacy and best online canadian pharmacy canadian discount pharmacy
purple pharmacy mexico price list mexican rx online or buying from online mexican pharmacy
http://markvierra.com/__media__/js/netsoltrademark.php?d=mexicoph.life> mexico drug stores pharmacies
best online pharmacies in mexico medication from mexico pharmacy and best online pharmacies in mexico mexico drug stores pharmacies
legitimate canadian pharmacy online: canada drugs direct – canadian pharmacies that deliver to the us
best online canadian pharmacy canadian family pharmacy or canadianpharmacymeds
http://diagpath.com/__media__/js/netsoltrademark.php?d=canadaph.life canadian drugs pharmacy
real canadian pharmacy canadian online pharmacy and canada rx pharmacy world canada discount pharmacy
stromectol ireland ivermectin price usa or ivermectin cost
http://crazywomanfudge.com/__media__/js/netsoltrademark.php?d=ivermectin.auction stromectol 12mg
buy ivermectin pills ivermectin 50 and stromectol without prescription stromectol for humans
ivermectin nz ivermectin over the counter canada or ivermectin oral
http://www.aiaindychapter.com/__media__/js/netsoltrademark.php?d=ivermectin.today stromectol drug
ivermectin stromectol ivermectin price comparison and cost of ivermectin cream ivermectin otc
ivermectin buy online ivermectin brand name or how much is ivermectin
http://chamber-mn.biz/__media__/js/netsoltrademark.php?d=ivermectin.today ivermectin over the counter canada
ivermectin 500mg can you buy stromectol over the counter and ivermectin 2mg ivermectin oral
ivermectin 9 mg ivermectin lotion for lice or ivermectin over the counter
http://bookiosk.com/__media__/js/netsoltrademark.php?d=ivermectin.today ivermectin 3
stromectol 6 mg tablet buy ivermectin cream and order stromectol ivermectin where to buy for humans
cost of ivermectin medicine purchase oral ivermectin or ivermectin price uk
http://istreaming.pro/__media__/js/netsoltrademark.php?d=ivermectinpharmacy.best ivermectin 400 mg brands
stromectol otc stromectol 3mg cost and ivermectin buy nz ivermectin usa
neurontin 200 mg capsules 32 neurontin or neurontin prescription coupon
http://microwaveaccessories.net/__media__/js/netsoltrademark.php?d=gabamed.store neurontin 202
neurontin price india neurontin medication and gabapentin medication 800mg neurontin
lasix online furosemide 40mg or lasix generic
http://spiritofnature.com/__media__/js/netsoltrademark.php?d=lasixfurosemide.store generic lasix
buy lasix online lasix 100 mg tablet and lasix lasix generic name
ivermectin lice ivermectin coronavirus or ivermectin where to buy for humans
http://reliablegeek.net/__media__/js/netsoltrademark.php?d=ivermectinpharmacy.best stromectol australia
stromectol ivermectin tablets stromectol how much it cost and ivermectin 2mg cost of stromectol medication
mexican online pharmacies prescription drugs: mexican online pharmacies prescription drugs – mexican drugstore online
reliable canadian online pharmacy canada ed drugs or canada pharmacy reviews
http://wholesalecondensers.com/__media__/js/netsoltrademark.php?d=canadaph.pro canadian pharmacy review
canadian drugs canadian pharmacy and canada drugs online canadian pharmacy
canada pharmacy online legit canadian pharmacy or canadian pharmacy no scripts
http://clickatellsucks.info/__media__/js/netsoltrademark.php?d=canadaph.pro canadian pharmacy online
canadian neighbor pharmacy canadian pharmacy online reviews and canadian pharmacy checker canadian online drugs
buy canadian drugs: certified online pharmacy canada – canadian pharmacy
buying prescription drugs in mexico online buying prescription drugs in mexico online or mexican online pharmacies prescription drugs
http://anadigics.at/__media__/js/netsoltrademark.php?d=mexicoph.icu mexico drug stores pharmacies
mexican rx online medicine in mexico pharmacies and purple pharmacy mexico price list buying from online mexican pharmacy
top 10 online pharmacy in india best online pharmacy india or top online pharmacy india
http://saveonpurchasing.com/__media__/js/netsoltrademark.php?d=indiaph.ink Online medicine order
india online pharmacy indianpharmacy com and top online pharmacy india indianpharmacy com
best online canadian pharmacy review canadian drug price checker buy rx online
best website to buy prescription drugs online pharmacy not requiring prescription or pharmacy canada
http://ww6.housesinteriors.com/__media__/js/netsoltrademark.php?d=interpharm.pro safe canadian pharmacies online
canadian drug stores best canadian drugstore and best us online pharmacy online pharmacy in india
prescription drugs canada rx mexico online or foi wesley chapel
http://nationstarrefinancing.org/__media__/js/netsoltrademark.php?d=internationalpharmacy.icu canadian pharmacy non prescription
online medicine without prescription online pharmacies without prescription and buy drugs online without a prescription canadian mail order pharmacies
mexican rx online us based online pharmacy or canada prescriptions by mail
http://medifaststcloudmn.com/__media__/js/netsoltrademark.php?d=internationalpharmacy.icu us online pharmacy reviews
best online mexican pharmacy best online pharmacy no prescription and prescription drugs online canada safe canadian pharmacies online
legit canadian pharmacy online candaian pharmacies or best online pharmacy that does not require a prescription in india
http://availa-zmc.com/__media__/js/netsoltrademark.php?d=interpharm.pro reviews of canadian online pharmacies
online canadian pharmacy pharmacy.com canada and canadian oharmacy canadianpharmacyonline
canadian rx store mexican pharmacies online or pharmacy in canada that ships to us
http://fashion-talent.com/__media__/js/netsoltrademark.php?d=internationalpharmacy.icu foreign pharmacies com
canadian neighborhood pharmacy online prescription canada and online india pharmacy canadian pharmecy
medications online without prescriptions best international online pharmacies or canada rx online
http://calrx.com/__media__/js/netsoltrademark.php?d=internationalpharmacy.icu canada pharmacy world
buy prescription drugs on line canadian pills and canadian mail order prescriptions pharmacy online india
http://interpharm.pro/# good online mexican pharmacy
cheap canadian drugs online – interpharm.pro Their pharmacists are top-notch; highly trained and personable.
www canadian pharmacies cheap prescription drugs online or online pharmacy canada no prescription
http://www.susanreinstein.com/__media__/js/netsoltrademark.php?d=internationalpharmacy.icu canadian online drug store
1 online worldwide drugstore online indian pharmacy and can you buy prescription drugs in canada pills no prescription
pharmacie ouverte Pharmacie en ligne pas cher or Pharmacie en ligne fiable
http://plustraffic.net/__media__/js/netsoltrademark.php?d=pharmacieenligne.icu pharmacie ouverte
Pharmacie en ligne sans ordonnance Pharmacie en ligne France and pharmacie ouverte 24/24 Acheter mГ©dicaments sans ordonnance sur internet
farmacia 24h farmacia online 24 horas or farmacias online seguras en espaГ±a
http://napervillequickcheck.org/__media__/js/netsoltrademark.php?d=farmaciabarata.pro farmacia online madrid
farmacias online baratas farmacia online madrid and farmacia barata farmacias baratas online envГo gratis
comprare farmaci online all’estero acquistare farmaci senza ricetta or farmacia online
http://greatlakesvisitorsguide.com/__media__/js/netsoltrademark.php?d=farmaciaonline.men п»їfarmacia online migliore
farmacia online farmacia online miglior prezzo and farmacia online migliore comprare farmaci online all’estero
https://pharmacieenligne.icu/# Pharmacie en ligne pas cher
farmacia 24h farmacia online barata farmacias baratas online envГo gratis
versandapotheke versandkostenfrei internet apotheke or online apotheke versandkostenfrei
http://cqn.ca/__media__/js/netsoltrademark.php?d=onlineapotheke.tech versandapotheke versandkostenfrei
versandapotheke versandkostenfrei online apotheke deutschland and versandapotheke deutschland online apotheke deutschland
https://farmaciaonline.men/# comprare farmaci online con ricetta
migliori farmacie online 2023 comprare farmaci online all’estero or farmacia online miglior prezzo
http://www.positiveperformance.com/__media__/js/netsoltrademark.php?d=farmaciaonline.men migliori farmacie online 2023
acquisto farmaci con ricetta farmacie online autorizzate elenco and migliori farmacie online 2023 farmacie online affidabili
Pharmacie en ligne pas cher Pharmacie en ligne pas cher or acheter mГ©dicaments Г l’Г©tranger
http://onedemand.net/__media__/js/netsoltrademark.php?d=pharmacieenligne.icu Acheter mГ©dicaments sans ordonnance sur internet
Pharmacie en ligne fiable п»їpharmacie en ligne and Pharmacie en ligne livraison 24h Pharmacie en ligne livraison 24h
https://onlineapotheke.tech/# gГјnstige online apotheke
farmacia envГos internacionales farmacia online barata or farmacia online 24 horas
http://brizofashionweek.com/__media__/js/netsoltrademark.php?d=farmaciabarata.pro farmacia online envГo gratis
farmacia barata farmacias online seguras en espaГ±a and п»їfarmacia online farmacias baratas online envГo gratis
farmaci senza ricetta elenco migliori farmacie online 2023 or farmacie online autorizzate elenco
http://davidweekleyhomesstink.org/__media__/js/netsoltrademark.php?d=itfarmacia.pro farmacia online miglior prezzo
farmaci senza ricetta elenco п»їfarmacia online migliore and acquistare farmaci senza ricetta farmacia online miglior prezzo
Viagra homme prix en pharmacie
http://edpharmacie.pro/# Pharmacies en ligne certifiГ©es
Viagra homme prix en pharmacie
pharmacie ouverte Pharmacie en ligne France or Pharmacie en ligne livraison rapide
http://yoursurance.com/__media__/js/netsoltrademark.php?d=edpharmacie.pro Pharmacies en ligne certifiГ©es
Pharmacie en ligne sans ordonnance Pharmacie en ligne France and п»їpharmacie en ligne Pharmacie en ligne fiable
https://edpharmacie.pro/# acheter medicament a l etranger sans ordonnance
farmacia online madrid farmacia online madrid or farmacia barata
http://www.fsp-llc.com/__media__/js/netsoltrademark.php?d=esfarmacia.men farmacia online 24 horas
farmacias online seguras п»їfarmacia online and farmacia online envГo gratis farmacia 24h
farmacie online autorizzate elenco farmacia online miglior prezzo or acquistare farmaci senza ricetta
http://abafoundry.biz/__media__/js/netsoltrademark.php?d=itfarmacia.pro acquistare farmaci senza ricetta
acquistare farmaci senza ricetta farmacia online miglior prezzo and farmacie online autorizzate elenco acquisto farmaci con ricetta
wonderful issues altogether, you just won a new reader. What could you suggest about your publish that you made a few days in the past? Any certain?
п»їbest mexican online pharmacies medicine in mexico pharmacies or mexican rx online
http://ohiosdairyfarmer.org/__media__/js/netsoltrademark.php?d=mexicopharm.store reputable mexican pharmacies online
mexican drugstore online mexican drugstore online and mexican online pharmacies prescription drugs buying prescription drugs in mexico
best canadian pharmacy online northwest canadian pharmacy or canadian pharmacy phone number
http://nationstarmortgageloans.info/__media__/js/netsoltrademark.php?d=canadapharm.store best canadian pharmacy to order from
canadian pharmacies comparison canadian pharmacy world and my canadian pharmacy reviews canadian pharmacy king reviews
cheapest pharmacy canada pet meds without vet prescription canada or canadian pharmacy online
http://gelriffic.net/__media__/js/netsoltrademark.php?d=canadapharm.store canada drugstore pharmacy rx
pharmacy wholesalers canada reputable canadian pharmacy and canadian pharmacy in canada canadapharmacyonline legit
We still cannot quite believe I would come to be those types of checking important points entirely on your webblog. My children i are sincerely thankful for ones generosity also giving me possibility pursue our chosen profession path. Information info I acquired of the web-site.
mexico pharmacies prescription drugs: mexican pharmaceuticals online – mexico drug stores pharmacies
india online pharmacy: Online medicine order – buy prescription drugs from india
Their private consultation rooms are a great addition. mail order pharmacy india: india pharmacy mail order – online pharmacy india
india pharmacy mail order reputable indian pharmacies or online pharmacy india
http://emaame.com/redir.cgi?url=https://indiapharm.cheap reputable indian online pharmacy
top 10 online pharmacy in india indianpharmacy com and indian pharmacy paypal mail order pharmacy india
online canadian drugstore pharmacy in canada or recommended canadian pharmacies
http://car-radio.net/__media__/js/netsoltrademark.php?d=canadapharm.store canadian pharmacy cheap
canada cloud pharmacy is canadian pharmacy legit and canadian pharmacies canadian neighbor pharmacy
buying prescription drugs in mexico: buying from online mexican pharmacy – mexico pharmacies prescription drugs
mexico drug stores pharmacies mexican rx online or mexican online pharmacies prescription drugs
http://joyousgifts.net/__media__/js/netsoltrademark.php?d=mexicopharm.store buying prescription drugs in mexico online
reputable mexican pharmacies online pharmacies in mexico that ship to usa and mexican border pharmacies shipping to usa best online pharmacies in mexico
I am glad to be one of several visitants on this great web site (:, regards for posting .
A trusted voice in global health matters. buying from online mexican pharmacy: mexican online pharmacies prescription drugs – mexico drug stores pharmacies
It’s best to participate in a contest for among the best blogs on the web. I’ll advocate this website!
After research a number of of the weblog posts on your web site now, and I really like your manner of blogging. I bookmarked it to my bookmark website record and will be checking back soon. Pls try my web site as effectively and let me know what you think.
You can also put a chatbox on your blog for more interactivity among readers.*.~;:
canadadrugpharmacy com: reputable canadian pharmacy – canadian pharmacy price checker
canadian compounding pharmacy online canadian pharmacy or canadianpharmacy com
http://batteryclinic.info/__media__/js/netsoltrademark.php?d=canadapharm.store canada pharmacy
canadian pharmacy review cheapest pharmacy canada and prescription drugs canada buy online canada ed drugs
canadian neighbor pharmacy: cheap canadian pharmacy – canada drug pharmacy
Drug information. indian pharmacy online: best india pharmacy – reputable indian pharmacies
best online pharmacy india buy prescription drugs from india or indian pharmacy online
http://sadar.net/__media__/js/netsoltrademark.php?d=indiapharm.cheap india pharmacy
Online medicine order п»їlegitimate online pharmacies india and Online medicine order indian pharmacy
my canadian pharmacy reviews canadian drugs online or canadian valley pharmacy
http://carcreditnc.com/__media__/js/netsoltrademark.php?d=canadapharm.store canada drugs reviews
canadian drugstore online canada pharmacy world and pharmacy canadian superstore legitimate canadian pharmacy
Prescription Drug Information, Interactions & Side. canadian pharmacy checker: canadian pharmacy store – onlinecanadianpharmacy
mexico pharmacies prescription drugs: п»їbest mexican online pharmacies – mexican pharmaceuticals online
п»їbest mexican online pharmacies mexico pharmacies prescription drugs or purple pharmacy mexico price list
http://abyvl.com/__media__/js/netsoltrademark.php?d=mexicopharm.store purple pharmacy mexico price list
mexican drugstore online mexico drug stores pharmacies and buying prescription drugs in mexico mexican rx online
buying drugs from canada my canadian pharmacy reviews or reliable canadian pharmacy
http://personalfinanceblog.com/__media__/js/netsoltrademark.php?d=canadapharm.store medication canadian pharmacy
canadian valley pharmacy canadian pharmacy review and best canadian pharmacy to order from canada rx pharmacy world
Their cross-border services are unmatched. vipps approved canadian online pharmacy: pharmacy canadian superstore – canadianpharmacy com
mexico pharmacies prescription drugs: п»їbest mexican online pharmacies – mexican online pharmacies prescription drugs
best rated canadian pharmacy online canadian drugstore or 77 canadian pharmacy
http://networksolutionsgroup.us/__media__/js/netsoltrademark.php?d=canadapharm.store reliable canadian online pharmacy
canada pharmacy reviews cheap canadian pharmacy and canadian pharmacy cheap canadian family pharmacy
pharmacy website india indianpharmacy com or world pharmacy india
http://activatemomentum.com/__media__/js/netsoltrademark.php?d=indiapharm.cheap/ top online pharmacy india
top 10 online pharmacy in india cheapest online pharmacy india and indian pharmacies safe world pharmacy india
onlinepharmaciescanada com: canada pharmacy online – legit canadian pharmacy
They’re globally renowned for their impeccable service. canadian pharmacy ltd: canadian pharmacy – canadian pharmacy scam
mexican drugstore online: best online pharmacies in mexico – pharmacies in mexico that ship to usa
mexican mail order pharmacies mexican mail order pharmacies or buying from online mexican pharmacy
http://jasonscience.org/__media__/js/netsoltrademark.php?d=mexicopharm.store mexican drugstore online
pharmacies in mexico that ship to usa mexican online pharmacies prescription drugs and medicine in mexico pharmacies buying from online mexican pharmacy
http://doxycyclineotc.store/# doxycycline brand name india
They always have valuable advice on medication management. http://azithromycinotc.store/# where can you buy zithromax
Their worldwide outreach programs are commendable. http://edpillsotc.store/# best ed pills
doxycycline 100mg coupon doxycycline prescription online or doxycycline 400 mg tablet
http://www.pageant-ppr.com/__media__/js/netsoltrademark.php?d=doxycyclineotc.store buying doxycycline uk
doxycycline online pharmacy canada doxycycline capsules india and doxycycline cap 50mg п»їdoxycycline 100mg tablets for sale
ed dysfunction treatment impotence pills or treatments for ed
http://portablesunlimited.biz/__media__/js/netsoltrademark.php?d=edpillsotc.store ed pills otc
buy erection pills top ed pills and erectile dysfunction medications best medication for ed
ed treatment pills buy erection pills or best ed pill
http://academysportsandoutdoor.net/__media__/js/netsoltrademark.php?d=edpillsotc.store best pills for ed
ed medications list treatment of ed and ed treatment pills erection pills online
medicine for erectile ed pills non prescription online ed pills
order zithromax without prescription cheap zithromax pills or zithromax 500mg over the counter
http://stopthewar.org/__media__/js/netsoltrademark.php?d=azithromycinotc.store how to get zithromax
where can i buy zithromax medicine zithromax over the counter canada and can you buy zithromax over the counter zithromax for sale usa
Been a loyal customer for years and they’ve never let me down. doxycycline 40 mg generic: buy doxycycline – where can i buy doxycycline capsules
Their global outlook is evident in their expansive services. http://azithromycinotc.store/# zithromax for sale online
I confirm. And I have faced it. Let’s discuss this question.
I’m impressed with their commitment to customer care. https://edpillsotc.store/# best ed pills online
While online gambling in Canada is growing in popularity, there is still plenty of demand for real casinos and traditional brick-and-mortar establishments. Some players prefer the excitement of attending a land-based casino compared to a casino online, while instant payouts are another big draw. West Virginia casino users can take advantage of a great promo at WV BetRivers where you will get $250 in covered losses during the first 24 hours. BetRivers offers a number of casino games including popular slots, blackjack, roulette, let it ride, and more. Click here to take advantage of this great welcome offer for new WV casino users. BetRivers Policy Even though BetMGM Sportsbook is live in New York, BetMGM New York Online Casino is not live, considering online casinos aren’t yet legal in the state. However, other live markets give a solid hint as to what the bonus offer from BetMGM might be if the online casino does go live in New York.
https://socialdosa.com/story4727083/euromillions-lotto-prediction
Aside from unlocking more pokies, you can also opt for Bonus doors and overcome the challenge of the naughty monkeys for coins and incredible prizes. What is more amazing about Wizard of Oz Slots games is that you can play along with your friends. You can also send some free presents for them if you want. 2.HappyMod App can continue downloading Wizard of Oz Slots Games Mod Apk 37.0.1430 APK from break point,no need to worry about reloading caused by interrupt. One of the highlights of Wizard of Oz Slots games is their visually stunning themes and designs. Each game within the franchise offers a unique aesthetic that captures the essence of different parts of the Oz universe. From the vibrant colors of Munchkinland to the eerie atmosphere of the Wicked Witch’s castle, players are treated to a feast for the eyes as they spin the reels.
i would love to use hydrogen fuel on my car, this fuel is really nonpolluting but is not yet very available*
buying ed pills online buy ed pills online medication for ed dysfunction
http://edpillsotc.store/# ed treatment drugs
indian pharmacy paypal indianpharmacy com or pharmacy website india
http://josephmanley.com/__media__/js/netsoltrademark.php?d=indianpharmacy.life п»їlegitimate online pharmacies india
indian pharmacy paypal best online pharmacy india and india pharmacy indian pharmacy online
They stock quality medications from all over the world. http://mexicanpharmacy.site/# purple pharmacy mexico price list
mexico pharmacies prescription drugs mexican border pharmacies shipping to usa or buying from online mexican pharmacy
http://lovepats.com/__media__/js/netsoltrademark.php?d=mexicanpharmacy.site п»їbest mexican online pharmacies
mexican drugstore online best online pharmacies in mexico and buying prescription drugs in mexico online mexico drug stores pharmacies
online pharmacy without scripts canadian pharmacy without prescription www pharmacyonline
online pharmacy indonesia my canadian pharmacy or online pharmacy worldwide shipping
http://vreturn.com/__media__/js/netsoltrademark.php?d=drugsotc.pro best online pharmacy usa
walmart online pharmacy canada drugs online review and canadian pharmacy coupon online canadian pharmacy coupon
A harmonious blend of local care and global expertise. http://mexicanpharmacy.site/# medication from mexico pharmacy
They’re at the forefront of international pharmaceutical innovations. https://drugsotc.pro/# 24 hour pharmacy near me
specialty pharmacy online pharmacy india or mail order pharmacy no prescription
http://vietnam-tourist.org/__media__/js/netsoltrademark.php?d=drugsotc.pro online pharmacy birth control pills
good online mexican pharmacy best online pharmacy usa and onlinecanadianpharmacy pharmacy home delivery
indian pharmacy indian pharmacy paypal or best online pharmacy india
http://mango-recruitment.com/__media__/js/netsoltrademark.php?d=indianpharmacy.life best online pharmacy india
top 10 online pharmacy in india п»їlegitimate online pharmacies india and indian pharmacy paypal world pharmacy india
Their global approach ensures unparalleled care. http://drugsotc.pro/# world pharmacy india
Their international partnerships enhance patient care. https://drugsotc.pro/# canadian pharmacy levitra value pack
best online pet pharmacy prescription drugs online or pharmacy online 365 discount code
http://sunyachts.biz/__media__/js/netsoltrademark.php?d=drugsotc.pro canada pharmacy coupon
canadian prescription pharmacy mexican pharmacy what to buy and www canadianonlinepharmacy trustworthy online pharmacy
mexican pharmaceuticals online buy drugs at mexican pharmacy pharmacies in mexico that ship to usa
mexican online pharmacies prescription drugs buying from online mexican pharmacy or purple pharmacy mexico price list
http://whatwouldmikesay.net/__media__/js/netsoltrademark.php?d=mexicanpharmacy.site mexican drugstore online
buying from online mexican pharmacy mexico pharmacies prescription drugs and medication from mexico pharmacy purple pharmacy mexico price list
Always professional, whether dealing domestically or internationally. http://indianpharmacy.life/# india pharmacy mail order
cheap online pharmacy my canadian pharmacy or drugs from canada
http://musclecarhotline.com/__media__/js/netsoltrademark.php?d=drugsotc.pro us pharmacy no prescription
best online pharmacy for viagra canadian pharmacy viagra 50 mg and canadian pharmacy sarasota pharmacy coupons
india pharmacy mail order canadian mail order pharmacy mexico pharmacy order online
canada drugs cost less pharmacy or my canadian pharmacy rx
http://oakgrove-70.info/__media__/js/netsoltrademark.php?d=drugsotc.pro buy online pharmacy uk
medstore online pharmacy buy drugs from canada and top 10 pharmacies in india canadian pharmacy india
reputable indian pharmacies indian pharmacy or best online pharmacy india
http://pickoneup.com/__media__/js/netsoltrademark.php?d=indianpharmacy.life reputable indian pharmacies
best india pharmacy indianpharmacy com and top 10 pharmacies in india reputable indian online pharmacy
canadian pharmacy tampa: pharmacy wholesalers canada – canadian pharmacy drugs online
canadien pharmacy indianpharmaonline review or buy canadian drugs online
http://paysageintime.com/__media__/js/netsoltrademark.php?d=internationalpharmacy.pro pharmacy canada online
online prescription canada top rated canadian pharmacy online and online pharmacy without prescription candain pharmacy
I appreciate their late hours for those unexpected needs. https://gabapentin.world/# neurontin 202
canadian drugs pharmacy legitimate canadian online pharmacies or the canadian pharmacy
http://valortel.net/__media__/js/netsoltrademark.php?d=canadapharmacy.cheap canada rx pharmacy
best canadian online pharmacy safe reliable canadian pharmacy and legit canadian pharmacy best canadian pharmacy
canada world pharmacy: mexican pharmacy without prescription – online pharmacy in india
cheap canadian pharmacy reddit canadian pharmacy or canadian drug stores
http://youngevityminerals.com/__media__/js/netsoltrademark.php?d=canadapharmacy.cheap canadian pharmacy no scripts
my canadian pharmacy rx canadian pharmacy no rx needed and online canadian pharmacy canadian online drugs
Always professional, whether dealing domestically or internationally. http://mexicanpharmonline.shop/# mexican online pharmacies prescription drugs
mexican mail order pharmacies mexico pharmacy medication from mexico pharmacy
mexico drug stores pharmacies and mexico pharmacy price list – mexican rx online
best online pharmacies in mexico buying prescription drugs in mexico online or mexican online pharmacies prescription drugs
http://adilkhan.com/__media__/js/netsoltrademark.php?d=mexicanpharmonline.shop medication from mexico pharmacy
mexico pharmacies prescription drugs medication from mexico pharmacy and pharmacies in mexico that ship to usa medication from mexico pharmacy
п»їbest mexican online pharmacies reputable mexican pharmacies online or mexican pharmaceuticals online
http://aabb.name/__media__/js/netsoltrademark.php?d=mexicanpharmonline.shop mexico pharmacies prescription drugs
buying prescription drugs in mexico mexico drug stores pharmacies and reputable mexican pharmacies online reputable mexican pharmacies online
medicine in mexico pharmacies mexico pharmacy or mexican drugstore online
http://securityworx.com/__media__/js/netsoltrademark.php?d=mexicanpharmonline.com medicine in mexico pharmacies
medication from mexico pharmacy mexico pharmacy and medication from mexico pharmacy mexico drug stores pharmacies
mexican drugstore online or mexico pharmacy online – buying prescription drugs in mexico
mexico drug stores pharmacies and mexico pharmacy – mexico pharmacies prescription drugs
Their health seminars are always enlightening. http://mexicanpharmonline.shop/# mexican border pharmacies shipping to usa
mexican pharmaceuticals online mexican pharmacy п»їbest mexican online pharmacies
Through which Article is stuffed with helpful. Many thanks for that kind connected to expressing C Follow through later on.
buying prescription drugs in mexico online : mexican pharmacy online – buying from online mexican pharmacy
mexican online pharmacies prescription drugs buying prescription drugs in mexico online or mexican pharmaceuticals online
http://boomerangvm.com/__media__/js/netsoltrademark.php?d=mexicanpharmonline.shop buying prescription drugs in mexico online
mexican online pharmacies prescription drugs п»їbest mexican online pharmacies and mexican drugstore online mexican rx online
They offer unparalleled advice on international healthcare. https://mexicanpharmonline.shop/# buying prescription drugs in mexico
medicine in mexico pharmacies mexico online pharmacy mexican mail order pharmacies
mexican pharmaceuticals online – mexico online pharmacy – mexican rx online
mexican mail order pharmacies or purple pharmacy mexico price list – buying prescription drugs in mexico
buying prescription drugs in mexico online mexican mail order pharmacies or best online pharmacies in mexico
http://romanticny.com/__media__/js/netsoltrademark.php?d=mexicanpharmonline.shop mexican border pharmacies shipping to usa
reputable mexican pharmacies online purple pharmacy mexico price list and mexico pharmacies prescription drugs mexican pharmaceuticals online
https://stromectol24.pro/# stromectol medicine
top 10 online pharmacy in india: india pharmacy – indian pharmacy online
canadian pharmacy meds canada drug pharmacy or canadian family pharmacy
http://engagementdinner.com/__media__/js/netsoltrademark.php?d=canadapharmacy24.pro precription drugs from canada
canadian pharmacy victoza canadian pharmacy com and my canadian pharmacy review northern pharmacy canada
http://indiapharmacy24.pro/# top 10 pharmacies in india
ivermectin 50mg/ml: ivermectin 5ml – ivermectin 1 cream
http://indiapharmacy24.pro/# indian pharmacies safe
indian pharmacy paypal india pharmacy or indian pharmacies safe
http://chinasurftour.cn/__media__/js/netsoltrademark.php?d=indiapharmacy24.pro top 10 pharmacies in india
indian pharmacy paypal mail order pharmacy india and reputable indian pharmacies п»їlegitimate online pharmacies india
canadian pharmacy no scripts: best pharmacy online – pharmacy rx world canada
Моментально возводимые здания: прибыль для бизнеса в каждой части!
В сегодняшнем обществе, где время имеет значение, строения быстрого монтажа стали истинным спасением для предпринимательства. Эти новейшие строения комбинируют в себе твердость, финансовую эффективность и ускоренную установку, что делает их отличным выбором для различных бизнес-проектов.
Металлоконструкции здания под ключ
1. Высокая скорость возвода: Секунды – самое ценное в коммерции, и экспресс-сооружения способствуют значительному сокращению сроков возведения. Это высоко оценивается в сценариях, когда срочно требуется начать бизнес и начать зарабатывать.
2. Финансовая эффективность: За счет совершенствования производственных процессов элементов и сборки на площадке, цена скоростроительных зданий часто оказывается ниже, по сопоставлению с традиционными строительными задачами. Это дает возможность сэкономить деньги и достичь более высокой инвестиционной доходности.
Подробнее на http://scholding.ru/
В заключение, моментальные сооружения – это идеальное решение для коммерческих инициатив. Они комбинируют в себе быстрое строительство, эффективное использование ресурсов и надежные характеристики, что позволяет им отличным выбором для предпринимателей, имеющих целью быстрый бизнес-старт и извлекать прибыль. Не упустите момент экономии времени и средств, прекрасно себя показавшие быстровозводимые сооружения для вашего следующего начинания!
Быстромонтажные здания: финансовая польза в каждой составляющей!
В современном мире, где минуты – капитал, быстровозводимые здания стали настоящим выходом для компаний. Эти современные объекты обладают надежность, экономичность и мгновенную сборку, что позволяет им лучшим выбором для коммерческих мероприятий.
Быстровозводимые конструкции недорого
1. Высокая скорость возвода: Моменты – наиважнейший аспект в бизнесе, и экспресс-сооружения обеспечивают существенное уменьшение сроков стройки. Это особенно ценно в ситуациях, когда срочно нужно начать бизнес и начать получать прибыль.
2. Финансовая выгода: За счет улучшения процессов изготовления элементов и сборки на объекте, расходы на скоростройки часто уменьшается, по сопоставлению с традиционными строительными задачами. Это позволяет сократить затраты и обеспечить более высокий доход с инвестиций.
Подробнее на http://scholding.ru
В заключение, скоростроительные сооружения – это первоклассное решение для предпринимательских задач. Они объединяют в себе эффективное строительство, бюджетность и долговечность, что придает им способность оптимальным решением для предприятий, активно нацеленных на скорый старт бизнеса и обеспечивать доход. Не упустите возможность получить выгоду в виде сэкономленного времени и денег, наилучшие объекты быстрого возвода для вашего следующего делового мероприятия!
minocycline antibiotic ivermectin 500mg or buy minocycline 50mg otc
http://ultimatefaceoff.com/__media__/js/netsoltrademark.php?d=stromectol24.pro stromectol pill for humans
where can i buy stromectol stromectol over the counter and minocycline for uti stromectol sales
http://stromectol24.pro/# ivermectin 0.1
canadian pharmacy reviews canada pharmacy reviews or my canadian pharmacy
http://www.microfundicion.net/__media__/js/netsoltrademark.php?d=canadapharmacy24.pro canadian discount pharmacy
canadian pharmacy 24h com safe canadian discount pharmacy and pharmacy in canada canadian pharmacy world
canadian pharmacy king: best pharmacy online – best canadian pharmacy
cost cheap mobic without a prescription: buy mobic – where to get cheap mobic without prescription
http://paxlovid.bid/# paxlovid covid
stromectol for humans buy minocycline 50 mg minocycline 100mg online
http://valtrex.auction/# buy generic valtrex without prescription
cost of valtrex in india valtrex tablets for sale or generic valtrex
http://moneyonebank.com/__media__/js/netsoltrademark.php?d=valtrex.auction paypal buy valtrex online canada
valtrex generic purchase valtrex online and valtrex generic in mexico valtrex cream
ivermectin cost is minocycline an antibiotic or stromectol xr
http://thinkactdo.com/__media__/js/netsoltrademark.php?d=stromectol.icu ivermectin 0.1 uk
ivermectin canada ivermectin 6mg dosage and ivermectin where to buy for humans buy ivermectin pills
buy paxlovid online: antiviral paxlovid pill – paxlovid cost without insurance
http://mobic.icu/# cost mobic online
stromectol uk buy ivermectin 24 mg ivermectin 5ml
п»їpaxlovid buy paxlovid online or paxlovid generic
http://dr724.com/__media__/js/netsoltrademark.php?d=paxlovid.bid Paxlovid buy online
paxlovid buy buy paxlovid online and paxlovid pharmacy paxlovid cost without insurance
Plavix generic price buy Clopidogrel over the counter or Plavix generic price
http://educateproject.com/__media__/js/netsoltrademark.php?d=plavix.guru buy plavix
clopidogrel bisulfate 75 mg Cost of Plavix without insurance and clopidogrel bisulfate 75 mg buy Clopidogrel over the counter
minocycline mr: ivermectin 0.1 uk – ivermectin 1
https://stromectol.icu/# minocycline for uti
buy clopidogrel online: п»їplavix generic – buy Clopidogrel over the counter
http://stromectol.icu/# buy ivermectin uk
ivermectin 3 mg tablet dosage purchase stromectol minocycline warnings
where to buy mobic without prescription: buy mobic – can i order mobic without prescription
http://stromectol.icu/# purchase stromectol online
valtrex 2000 mg: generic valtrex best price – canadian valtrex no rx
п»їpaxlovid paxlovid india or paxlovid pill
http://www.hydorwellness.it/__media__/js/netsoltrademark.php?d=paxlovid.bid paxlovid cost without insurance
Paxlovid over the counter Paxlovid over the counter and paxlovid for sale paxlovid cost without insurance
valtrex discount how to get valtrex without a prescription or valtrex online no prescription
http://publicadvocatesinc.com/__media__/js/netsoltrademark.php?d=valtrex.auction valtrex online canada
valtrex online australia can you purchase valtrex online and valtrex 500mg online valtrex cost
where can i buy stromectol ivermectin 0.5 or order minocycline 50mg online
http://stv-boutique.com/__media__/js/netsoltrademark.php?d=stromectol.icu minocycline 50mg tabs
minocycline 50 mg tablet ivermectin rx and minocycline 50 mg pills online stromectol 3 mg tablet price
п»їplavix generic: cheap plavix antiplatelet drug – buy clopidogrel online
http://valtrex.auction/# buy valtrex
п»їplavix generic Cost of Plavix without insurance buy clopidogrel online
https://mobic.icu/# where buy cheap mobic without a prescription
ivermectin 50mg/ml: ivermectin usa price – stromectol price uk
generic plavix cheap plavix antiplatelet drug or buy Clopidogrel over the counter
http://kashmirgem.com/__media__/js/netsoltrademark.php?d=plavix.guru Cost of Plavix on Medicare
Cost of Plavix on Medicare Clopidogrel 75 MG price and generic plavix cheap plavix antiplatelet drug
Buy Tadalafil 20mg: Cheap Cialis – Cialis 20mg price in USA
Kamagra 100mg price sildenafil oral jelly 100mg kamagra buy Kamagra
http://kamagra.icu/# super kamagra
Cheap generic Viagra cheapest viagra or generic sildenafil
http://accountantstoday.com/__media__/js/netsoltrademark.php?d=viagra.eus Cheap Viagra 100mg
Generic Viagra for sale buy viagra here and Viagra tablet online buy viagra here
https://cialis.foundation/# cheapest cialis
Buy Tadalafil 20mg Cialis without a doctor prescription or cheapest cialis
http://vengeancefilms.com/__media__/js/netsoltrademark.php?d=cialis.foundation Generic Tadalafil 20mg price
Cialis without a doctor prescription Buy Tadalafil 10mg and Cheap Cialis Buy Cialis online
п»їkamagra п»їkamagra or Kamagra 100mg price
http://www.orbit3d.com/__media__/js/netsoltrademark.php?d=kamagra.icu Kamagra 100mg
buy kamagra online usa п»їkamagra and Kamagra Oral Jelly cheap kamagra
http://viagra.eus/# Cheap Viagra 100mg
Levitra 20 mg for sale Levitra 20 mg for sale Buy Vardenafil 20mg
http://viagra.eus/# Buy generic 100mg Viagra online
http://kamagra.icu/# super kamagra
Kamagra 100mg price cheap kamagra super kamagra
http://viagra.eus/# Viagra without a doctor prescription Canada
Cialis 20mg price cheapest cialis or Generic Cialis without a doctor prescription
http://ticklebugs.org/__media__/js/netsoltrademark.php?d=cialis.foundation buy cialis pill
п»їcialis generic Buy Tadalafil 20mg and Tadalafil Tablet Cialis 20mg price in USA
Generic Viagra for sale Sildenafil Citrate Tablets 100mg or Cheap generic Viagra online
http://christianguevara.com/__media__/js/netsoltrademark.php?d=viagra.eus generic sildenafil
Viagra Tablet price Sildenafil 100mg price and Sildenafil Citrate Tablets 100mg Viagra online price
https://kamagra.icu/# Kamagra Oral Jelly
Cheap Levitra online Buy Vardenafil online Cheap Levitra online
https://viagra.eus/# Generic Viagra for sale
https://kamagra.icu/# Kamagra 100mg price
п»їkamagra buy Kamagra sildenafil oral jelly 100mg kamagra
https://levitra.eus/# Cheap Levitra online
https://kamagra.icu/# п»їkamagra
buy cialis pill Buy Cialis online or Cialis without a doctor prescription
http://dreamit-buildit.net/__media__/js/netsoltrademark.php?d=cialis.foundation Buy Tadalafil 20mg
Generic Cialis without a doctor prescription Cheap Cialis and Tadalafil price Buy Tadalafil 5mg
sildenafil online sildenafil over the counter or Sildenafil 100mg price
http://barnonemortgage.com/__media__/js/netsoltrademark.php?d=viagra.eus cheapest viagra
viagra without prescription Cheap generic Viagra and Viagra online price Order Viagra 50 mg online
cialis for sale Buy Tadalafil 10mg Generic Cialis without a doctor prescription
http://levitra.eus/# Buy Vardenafil 20mg
https://kamagra.icu/# sildenafil oral jelly 100mg kamagra
Buy Tadalafil 5mg cheapest cialis Buy Cialis online
cheapest cialis Buy Tadalafil 10mg or Generic Cialis without a doctor prescription
http://workgearheadquarters.com/__media__/js/netsoltrademark.php?d=cialis.foundation Buy Tadalafil 10mg
Cialis 20mg price in USA Tadalafil Tablet and Cialis 20mg price in USA Generic Tadalafil 20mg price
https://cialis.foundation/# п»їcialis generic
http://kamagra.icu/# Kamagra tablets
canadian pharmacy india: indian pharmacy – online shopping pharmacy india indiapharmacy.pro
best online pharmacy india best india pharmacy mail order pharmacy india indiapharmacy.pro
https://indiapharmacy.pro/# cheapest online pharmacy india indiapharmacy.pro
mexico pharmacy: mexico pharmacy – mexican pharmaceuticals online mexicanpharmacy.company
canadian family pharmacy: canadian pharmacy king – safe reliable canadian pharmacy canadapharmacy.guru
п»їlegitimate online pharmacies india: buy prescription drugs from india – best india pharmacy indiapharmacy.pro
buy prescription drugs from india indianpharmacy com indian pharmacy indiapharmacy.pro
http://indiapharmacy.pro/# buy prescription drugs from india indiapharmacy.pro
canadian pharmacy meds: canadian pharmacy meds – legal to buy prescription drugs from canada canadapharmacy.guru
best online pharmacy india: cheapest online pharmacy india – indian pharmacy online indiapharmacy.pro
cheapest online pharmacy india buy prescription drugs from india best online pharmacy india indiapharmacy.pro
canadian neighbor pharmacy canadian pharmacy 24h com or canada drug pharmacy
http://alcocomfortclassic.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru canadian world pharmacy
online pharmacy canada canadian pharmacy tampa and canadian pharmacy meds cheapest pharmacy canada
Online medicine order: india pharmacy – best online pharmacy india indiapharmacy.pro
http://canadapharmacy.guru/# canada drugstore pharmacy rx canadapharmacy.guru
india pharmacy cheapest online pharmacy india or india pharmacy mail order
http://job-applications.net/__media__/js/netsoltrademark.php?d=indiapharmacy.pro world pharmacy india
india pharmacy india pharmacy mail order and reputable indian pharmacies world pharmacy india
top 10 pharmacies in india: best india pharmacy – india online pharmacy indiapharmacy.pro
mexico drug stores pharmacies reputable mexican pharmacies online buying prescription drugs in mexico mexicanpharmacy.company
online shopping pharmacy india: reputable indian pharmacies – pharmacy website india indiapharmacy.pro
canada drugs reviews canadian pharmacy ratings or legit canadian pharmacy
http://jlbjo.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru canada drugs online
pharmacy canadian ed meds online canada and recommended canadian pharmacies global pharmacy canada
canadianpharmacyworld com: canadapharmacyonline legit – canadian pharmacy canadapharmacy.guru
mexican border pharmacies shipping to usa mexican pharmaceuticals online medication from mexico pharmacy mexicanpharmacy.company
mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa or mexican drugstore online
http://cutiescorner.com/__media__/js/netsoltrademark.php?d=mexicanpharmacy.company mexico pharmacies prescription drugs
mexico drug stores pharmacies mexico drug stores pharmacies and buying prescription drugs in mexico online mexico drug stores pharmacies
http://indiapharmacy.pro/# buy prescription drugs from india indiapharmacy.pro
https://canadapharmacy.guru/# buy drugs from canada canadapharmacy.guru
canada discount pharmacy: pharmacies in canada that ship to the us – canadian pharmacy no rx needed canadapharmacy.guru
top 10 online pharmacy in india: indian pharmacy paypal – indian pharmacy indiapharmacy.pro
canadian king pharmacy canadian pharmacy 24h com or certified canadian international pharmacy
http://glendoravolvo.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru best online canadian pharmacy
canadian pharmacy com legitimate canadian mail order pharmacy and canadian world pharmacy canada drug pharmacy
best india pharmacy online shopping pharmacy india or indian pharmacy paypal
http://bearriverproduce.com/__media__/js/netsoltrademark.php?d=indiapharmacy.pro online pharmacy india
indian pharmacy paypal buy prescription drugs from india and top 10 pharmacies in india cheapest online pharmacy india
mexican rx online: mexican drugstore online – best online pharmacies in mexico mexicanpharmacy.company
mexican online pharmacies prescription drugs mexican pharmaceuticals online mexico drug stores pharmacies mexicanpharmacy.company
https://canadapharmacy.guru/# canadian pharmacies that deliver to the us canadapharmacy.guru
mexican drugstore online: buying prescription drugs in mexico – medicine in mexico pharmacies mexicanpharmacy.company
canada pharmacy online legit: canadian pharmacy online – pharmacy wholesalers canada canadapharmacy.guru
legit canadian pharmacy online best rated canadian pharmacy canadian pharmacy no rx needed canadapharmacy.guru
mexico pharmacy: medicine in mexico pharmacies – mexico pharmacy mexicanpharmacy.company
http://indiapharmacy.pro/# indian pharmacy online indiapharmacy.pro
medication from mexico pharmacy mexico drug stores pharmacies or mexican pharmaceuticals online
http://www.357ryderz.net/__media__/js/netsoltrademark.php?d=mexicanpharmacy.company mexican border pharmacies shipping to usa
mexico drug stores pharmacies pharmacies in mexico that ship to usa and buying from online mexican pharmacy п»їbest mexican online pharmacies
http://canadapharmacy.guru/# canadian pharmacy 365 canadapharmacy.guru
canada drugs canadian pharmacy online or reputable canadian pharmacy
http://beatinglupus.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru best mail order pharmacy canada
onlinecanadianpharmacy canadian mail order pharmacy and canada drugs online reviews online canadian drugstore
indian pharmacy online cheapest online pharmacy india or pharmacy website india
http://netexchangeservices.org/__media__/js/netsoltrademark.php?d=indiapharmacy.pro world pharmacy india
online pharmacy india indianpharmacy com and india pharmacy mail order world pharmacy india
india pharmacy: Online medicine order – india pharmacy mail order indiapharmacy.pro
india pharmacy mail order: cheapest online pharmacy india – top 10 pharmacies in india indiapharmacy.pro
buying from online mexican pharmacy mexico drug stores pharmacies mexico drug stores pharmacies mexicanpharmacy.company
legal canadian pharmacy online canadian pharmacy ratings or canadian pharmacy 24
http://www.multiplelistingservice.cc/__media__/js/netsoltrademark.php?d=canadapharmacy.guru pharmacy canadian superstore
canadian drug pharmacy canadian pharmacy king reviews and canadian pharmacy oxycodone canada drug pharmacy
http://indiapharmacy.pro/# indian pharmacy indiapharmacy.pro
canadian pharmacy oxycodone: best canadian pharmacy online – canadian pharmacy 365 canadapharmacy.guru
buying prescription drugs in mexico: mexico drug stores pharmacies – purple pharmacy mexico price list mexicanpharmacy.company
mexican online pharmacies prescription drugs: medication from mexico pharmacy – purple pharmacy mexico price list mexicanpharmacy.company
mexican mail order pharmacies mexico drug stores pharmacies mexican border pharmacies shipping to usa mexicanpharmacy.company
https://canadapharmacy.guru/# canadian drugs pharmacy canadapharmacy.guru
mexico drug stores pharmacies mexican rx online or best online pharmacies in mexico
http://bluffmfg.biz/__media__/js/netsoltrademark.php?d=mexicanpharmacy.company mexican online pharmacies prescription drugs
mexican mail order pharmacies medication from mexico pharmacy and mexico drug stores pharmacies reputable mexican pharmacies online
https://canadapharmacy.guru/# canadian pharmacy no scripts canadapharmacy.guru
buy medicines online in india indianpharmacy com or best india pharmacy
http://www.playingforareason.com/__media__/js/netsoltrademark.php?d=indiapharmacy.pro top online pharmacy india
indian pharmacy paypal best online pharmacy india and top 10 online pharmacy in india indian pharmacies safe
legit canadian online pharmacy: canada online pharmacy – canadian valley pharmacy canadapharmacy.guru
canadian pharmacies reputable canadian online pharmacies or online canadian pharmacy review
http://northshorepizza.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru pharmacy rx world canada
canadian pharmacy canada rx pharmacy world and canadian online pharmacy canada pharmacy reviews
canadadrugpharmacy com: onlinecanadianpharmacy 24 – buy prescription drugs from canada cheap canadapharmacy.guru
buy prescription drugs from india india pharmacy indian pharmacies safe indiapharmacy.pro
http://indiapharmacy.pro/# pharmacy website india indiapharmacy.pro
canadian pharmacy canadian pharmacy meds or best canadian online pharmacy reviews
http://umcevangelism.org/__media__/js/netsoltrademark.php?d=canadapharmacy.guru pharmacy com canada
ed drugs online from canada canadian family pharmacy and reputable canadian online pharmacy precription drugs from canada
mexico pharmacies prescription drugs: buying prescription drugs in mexico online – purple pharmacy mexico price list mexicanpharmacy.company
canadian pharmacy world reviews: canadian pharmacy no scripts – canadian pharmacy king reviews canadapharmacy.guru
pharmacies in mexico that ship to usa reputable mexican pharmacies online pharmacies in mexico that ship to usa mexicanpharmacy.company
pharmacies in mexico that ship to usa: buying prescription drugs in mexico – reputable mexican pharmacies online mexicanpharmacy.company
http://canadapharmacy.guru/# canadian online pharmacy canadapharmacy.guru
best online pharmacies in mexico mexican mail order pharmacies or mexican online pharmacies prescription drugs
http://availa-zmc.com/__media__/js/netsoltrademark.php?d=mexicanpharmacy.company mexican mail order pharmacies
mexican border pharmacies shipping to usa buying prescription drugs in mexico online and п»їbest mexican online pharmacies reputable mexican pharmacies online
world pharmacy india indianpharmacy com or indian pharmacies safe
http://tenniseverywhere.tv/__media__/js/netsoltrademark.php?d=indiapharmacy.pro top 10 pharmacies in india
top 10 pharmacies in india india pharmacy mail order and best online pharmacy india canadian pharmacy india
https://indiapharmacy.pro/# cheapest online pharmacy india indiapharmacy.pro
mail order pharmacy india: buy prescription drugs from india – best online pharmacy india indiapharmacy.pro
purple pharmacy mexico price list mexican border pharmacies shipping to usa buying prescription drugs in mexico online mexicanpharmacy.company
best online pharmacy india: best online pharmacy india – indian pharmacy paypal indiapharmacy.pro
https://mexicanpharmacy.company/# best online pharmacies in mexico mexicanpharmacy.company
pharmacies in mexico that ship to usa: mexico pharmacies prescription drugs – п»їbest mexican online pharmacies mexicanpharmacy.company
online canadian pharmacy canadian pharmacy service or canadian family pharmacy
http://folkmusichalloffame.com/__media__/js/netsoltrademark.php?d=canadapharmacy.guru canadian pharmacies that deliver to the us
thecanadianpharmacy canadian pharmacy meds review and canadian pharmacy 1 internet online drugstore canadian pharmacy in canada
online canadian pharmacy my canadian pharmacy reviews or reputable canadian pharmacy
http://carmenmedia.net/__media__/js/netsoltrademark.php?d=canadapharmacy.guru vipps approved canadian online pharmacy
canadian drugs legit canadian online pharmacy and best rated canadian pharmacy canadian online drugstore
п»їbest mexican online pharmacies: п»їbest mexican online pharmacies – buying from online mexican pharmacy mexicanpharmacy.company
mexican online pharmacies prescription drugs mexican online pharmacies prescription drugs mexico pharmacies prescription drugs mexicanpharmacy.company
https://indiapharmacy.pro/# india online pharmacy indiapharmacy.pro
indian pharmacies safe: best online pharmacy india – buy prescription drugs from india indiapharmacy.pro
top 10 pharmacies in india indian pharmacies safe or indianpharmacy com
http://ihatelaurel-scion.com/__media__/js/netsoltrademark.php?d=indiapharmacy.pro best online pharmacy india
indian pharmacy paypal п»їlegitimate online pharmacies india and top 10 online pharmacy in india buy medicines online in india
purple pharmacy mexico price list mexican drugstore online or mexican border pharmacies shipping to usa
http://cleverglobalnetwork.net/__media__/js/netsoltrademark.php?d=mexicanpharmacy.company medicine in mexico pharmacies
mexican online pharmacies prescription drugs buying from online mexican pharmacy and mexico drug stores pharmacies reputable mexican pharmacies online
doxycycline medication: where to purchase doxycycline – doxycycline order online
http://amoxil.world/# where to buy amoxicillin
order cheap propecia without insurance buy propecia without a prescription cost generic propecia for sale
can i order clomid online: get clomid tablets – where buy clomid pills
https://amoxil.world/# amoxicillin pharmacy price
http://prednisone.digital/# prednisone 2 mg daily
how to get clomid price can i buy cheap clomid price cheap clomid prices
how can i order prednisone: prednisone 20mg price in india – buying prednisone mexico
https://propecia.sbs/# order cheap propecia without dr prescription
http://prednisone.digital/# 5 prednisone in mexico
prednisone 20 mg tablet prednisone 1 mg daily prednisone drug costs
http://doxycycline.sbs/# where to get doxycycline
prednisone 20mg online no prescription online prednisone or prednisone online for sale
https://images.google.com.py/url?q=https://prednisone.digital prednisone uk buy
prednisone 21 pack prednisone buy online nz and purchase prednisone buy prednisone without a prescription
cost of cheap propecia: propecia otc – cost propecia prices
cheap clomid pills: can i order clomid pill – buying clomid without dr prescription
http://propecia.sbs/# generic propecia pill
amoxicillin 1000 mg capsule amoxicillin generic price for amoxicillin 875 mg
how to get clomid pills: where to buy clomid tablets – buying clomid prices
amoxicillin cost australia amoxicillin 500 mg purchase without prescription or purchase amoxicillin online
http://specials.moulinex.de/php/products/product.php?pid=100550&mlx-hst=www.amoxil.world&mlx-pi=/products/fryers/bineoproducts.aspx&family=fryers generic amoxicillin
amoxicillin order online no prescription amoxicillin without a prescription and amoxicillin 500mg where can i get amoxicillin
http://doxycycline.sbs/# 200 mg doxycycline
order propecia pills cheap propecia price or cost propecia without dr prescription
https://cse.google.com.ph/url?q=https://propecia.sbs cost of propecia without prescription
buy cheap propecia online propecia otc and buy propecia no prescription cost cheap propecia tablets
order generic propecia without dr prescription: buying cheap propecia without insurance – order generic propecia without dr prescription
http://amoxil.world/# order amoxicillin no prescription
where can i buy amoxicillin over the counter uk can i buy amoxicillin over the counter in australia amoxicillin 500 mg without a prescription
http://doxycycline.sbs/# doxycycline without a prescription
doxycycline 100mg capsules: cheap doxycycline online – generic for doxycycline
https://clomid.sbs/# buying cheap clomid online
buy doxycycline online uk doxycycline pills price of doxycycline
amoxicillin tablets in india amoxicillin 500mg capsules or amoxicillin 500mg for sale uk
https://wiki.ood.ch/api.php?action=https://amoxil.world amoxicillin azithromycin
where to buy amoxicillin purchase amoxicillin 500 mg and where to buy amoxicillin 500mg cheap amoxicillin 500mg
cost generic propecia without rx buy propecia online or get generic propecia without insurance
http://www.voidstar.com/opml/?url=http://propecia.sbs/ get cheap propecia without insurance
propecia cheap get cheap propecia no prescription and cost of propecia tablets order generic propecia for sale
http://amoxil.world/# amoxicillin 500mg price
http://clomid.sbs/# clomid tablets
buy prednisone without prescription paypal prednisone cost canada 20 mg of prednisone
prescription for amoxicillin: amoxicillin online without prescription – amoxicillin for sale
http://doxycycline.sbs/# odering doxycycline
http://doxycycline.sbs/# buy doxycycline 100mg
1250 mg prednisone prednisone 4mg tab can you buy prednisone over the counter in canada
get cheap clomid pills: order generic clomid pills – where to get cheap clomid without a prescription
amoxicillin 500mg for sale uk buying amoxicillin in mexico or buy amoxil
https://toolbarqueries.google.ad/url?q=http://amoxil.world amoxicillin 500 mg
where can i buy amoxicillin without prec generic amoxicillin and amoxicillin no prescription where can i buy amoxicillin online
https://amoxil.world/# where can you get amoxicillin
generic over the counter prednisone prednisone brand name in usa prednisone tablets india
propecia cheap cost of generic propecia price or buying propecia without prescription
https://images.google.nu/url?sa=t&url=https://propecia.sbs buy cheap propecia without rx
buy cheap propecia without a prescription cost of generic propecia online and cost propecia buy propecia no prescription
http://amoxil.world/# amoxicillin 500mg price
prednisone online india: order prednisone 100g online without prescription – 5 mg prednisone daily
how to get prescription drugs without doctor: prescription drugs without doctor approval – prescription drugs online without doctor
http://edpills.icu/# cheapest ed pills
http://indiapharm.guru/# indian pharmacy
online shopping pharmacy india best online pharmacy india online pharmacy india
buy prescription drugs without doctor: viagra without doctor prescription – 100mg viagra without a doctor prescription
https://canadapharm.top/# legit canadian pharmacy
https://canadapharm.top/# canadian mail order pharmacy
non prescription erection pills erection pills buy erection pills
best male enhancement pills: generic ed pills – generic ed drugs
compare ed drugs medicine erectile dysfunction or treatments for ed
https://stjohns.harrow.sch.uk/brighton-hove/primary/westdene/arenas/schooloffice/calendar/CookiePolicy.action?backto=https://edpills.icu non prescription erection pills
medications for ed top ed drugs and gnc ed pills best pills for ed
meds online without doctor prescription best non prescription ed pills or non prescription ed pills
https://maps.google.dm/url?q=https://withoutprescription.guru prescription drugs canada buy online
levitra without a doctor prescription prescription drugs and viagra without doctor prescription buy prescription drugs online
http://edpills.icu/# medicine for erectile
buy prescription drugs from india mexican pharmacy without prescription viagra without a doctor prescription
https://edpills.icu/# top rated ed pills
http://withoutprescription.guru/# prescription drugs online without doctor
п»їbest mexican online pharmacies: reputable mexican pharmacies online – mexico drug stores pharmacies
best online pharmacies in mexico mexican mail order pharmacies or buying prescription drugs in mexico
https://clients1.google.com.tn/url?q=http://mexicopharm.shop п»їbest mexican online pharmacies
mexican mail order pharmacies mexican drugstore online and medicine in mexico pharmacies buying prescription drugs in mexico
canadian pharmacy online reputable canadian pharmacy or onlinepharmaciescanada com
https://www.google.cv/url?sa=t&url=https://canadapharm.top canadian pharmacy tampa
canadian drug pharmacy canadian pharmacy service and canadian discount pharmacy canadian pharmacy oxycodone
http://edpills.icu/# best drug for ed
legal to buy prescription drugs without prescription discount prescription drugs ed prescription drugs
http://mexicopharm.shop/# purple pharmacy mexico price list
viagra without doctor prescription buy prescription drugs online or buy prescription drugs from canada cheap
http://www.wangxiao.cn/redirect.aspx?url=https://withoutprescription.guru/ discount prescription drugs
discount prescription drugs ed meds online without doctor prescription and viagra without a prescription ed meds online without doctor prescription
top 10 online pharmacy in india: indian pharmacies safe – india online pharmacy
compare ed drugs best ed drug or the best ed pills
https://justplayhere.com/proxy.php?link=https://edpills.icu best ed drug
new treatments for ed cheapest ed pills and ed pills otc ed pills that really work
http://canadapharm.top/# my canadian pharmacy review
non prescription ed pills buy prescription drugs from canada cheap buy prescription drugs from canada cheap
http://canadapharm.top/# legitimate canadian mail order pharmacy
reputable indian online pharmacy: reputable indian pharmacies – top online pharmacy india
mexican drugstore online: mexican rx online – mexico drug stores pharmacies
amoxicillin 500mg capsules antibiotic: amoxicillin online pharmacy – amoxicillin 500 mg tablet
viagra without doctor prescription prescription drugs without doctor approval or prescription meds without the prescriptions
http://nun.nu/withoutprescription.guru 100mg viagra without a doctor prescription
cialis without a doctor’s prescription cialis without doctor prescription and prescription drugs online ed meds online without doctor prescription
http://canadapharm.top/# canadian pharmacy antibiotics
canadapharmacyonline legit canadadrugpharmacy com or canadian pharmacy 24 com
http://trackroad.com/conn/garminimport.aspx?returnurl=https://canadapharm.top legit canadian pharmacy online
canada pharmacy pharmacies in canada that ship to the us and precription drugs from canada reliable canadian pharmacy
https://indiapharm.guru/# online pharmacy india
reputable mexican pharmacies online buying prescription drugs in mexico online medicine in mexico pharmacies
online prescription for ed meds: buy prescription drugs from canada cheap – discount prescription drugs
amoxicillin tablets in india: amoxicillin 500 mg capsule – amoxicillin 250 mg
purple pharmacy mexico price list mexico drug stores pharmacies or purple pharmacy mexico price list
https://cse.google.com.pg/url?sa=t&url=https://mexicopharm.shop mexican border pharmacies shipping to usa
buying from online mexican pharmacy mexican online pharmacies prescription drugs and mexico drug stores pharmacies buying prescription drugs in mexico
ed meds online without doctor prescription male ed pills or ed treatment review
http://ethr.net/phpinfo.php?a=<a+href=http://edpills.icu cheap ed drugs
ed medications list ed pills online and best ed pills online best otc ed pills
http://mexicopharm.shop/# mexican pharmaceuticals online
online ed pills the best ed pills best ed pills non prescription
ed meds online without doctor prescription: best ed pills – ed pills gnc
best non prescription ed pills: cialis without doctor prescription – ed meds online without doctor prescription
https://withoutprescription.guru/# levitra without a doctor prescription
Buy generic Levitra online: Vardenafil buy online – Cheap Levitra online
http://tadalafil.trade/# tadalafil tablets 20 mg buy
https://kamagra.team/# Kamagra 100mg
cheap kamagra Kamagra tablets Kamagra tablets
ed drugs: ed treatment pills – best ed pills non prescription
Kamagra 100mg price Kamagra Oral Jelly or Kamagra 100mg price
https://www.google.com.om/url?q=https://kamagra.team Kamagra 100mg
Kamagra Oral Jelly cheap kamagra and Kamagra 100mg price super kamagra
gnc ed pills ed drug prices or how to cure ed
https://maps.google.ht/url?q=https://edpills.monster erectile dysfunction medications
=how+can+i+buy+viagra]best drug for ed treatment for ed and best over the counter ed pills best pill for ed
sildenafil oral jelly 100mg kamagra sildenafil oral jelly 100mg kamagra sildenafil oral jelly 100mg kamagra
sildenafil oral jelly 100mg kamagra: Kamagra 100mg – cheap kamagra
sildenafil 20 mg tablets price sildenafil citrate tablets 100 mg or where can i buy sildenafil 20mg
http://clients1.google.mk/url?q=https://sildenafil.win order sildenafil online usa
sildenafil 48 tabs 50 mg price cheap sildenafil tablets and sildenafil 500 mg 20 mg sildenafil cost
tadalafil price uk: generic cialis tadalafil – 60 mg tadalafil
https://kamagra.team/# sildenafil oral jelly 100mg kamagra
https://kamagra.team/# super kamagra
tadalafil 2.5 mg tablets buy tadalafil over the counter or order tadalafil 20mg
https://www.google.vu/url?sa=t&url=https://tadalafil.trade tadalafil 10 mg canadian pharmacy
tadalafil online prescription buy tadalafil online paypal and tadalafil 20mg lowest price tadalafil 5mg tablets price
ed treatment review natural remedies for ed erection pills that work
erectile dysfunction medicines: ed medications online – ed pills otc
п»їkamagra cheap kamagra or Kamagra 100mg
https://maps.google.com.ng/url?q=https://kamagra.team cheap kamagra
cheap kamagra Kamagra 100mg price and Kamagra 100mg buy kamagra online usa
erection pills that work ed pills for sale ed pills comparison
tadalafil tablets 20 mg online: buy tadalafil 20 – 10mg tadalafil
At the moment you will find over 200 different Jackpot Slots at Pokerstars Casino. You won’t have to install any software to play these games (instant play). Because of this you can start spinning your favourite Jackpot Slot right after making your first deposit. And during every spin you will have a chance of winning one of the many amazing Jackpots. Below you will find some of the most popular Jackpot Slots that are currently available to play at Pokerstars Casino; Access industry-leading operators and brands within our rapidly growing network The jackpot bonuses can be won with any bet, but bigger spins can result in better odds. Divine Fortune has multiple ways to earn extra spins, but the most important is the “Falling Wild” Pegasus symbols. These wilds stay on the reel, moving one spot down while you get an extra spin. If you are lucky enough to spin another wild on this space, it becomes a “Wild on Wild” in which the Pegasus is spread out across all three rows of that reel (at least three more spins with wilds remaining on the field).
https://direct-wiki.win/index.php?title=Lucky_slots_casino_real_money
While Slotomania collects personal information in order to set up your account, this is kept private, and never sold on or disclosed to third parties. Slotomania may use your information to keep you informed about updates and special promotions to improve your gaming experience, but you may opt out of these communications whenever you wish. When it comes to playing via a social network, Slotomania only operates on the most prominent and trustworthy sites, such as Facebook and Twitter. An Slotomania original slot game filled with Multi-Reel Free Spins that unlock with EVERY puzzle you complete! Spin for pieces and complete puzzles for happy paws and lots of wins! A video shared from Aria’s casino reveals numerous gaming machines with blacked-out screens displaying an “out of service” message. Another clip showcases malfunctioning Aria slots with flickering screens, clearly indicating a software problem.
sildenafil tabs 20mg sildenafil cost uk or sildenafil in europe
https://todosobrelaesquizofrenia.com/Redirect/?url=https://sildenafil.win/ sildenafil 25 mg buy
buy cheap sildenafil uk sildenafil soft tabs generic and sildenafil tablets 100mg price sildenafil citrate tablets 100 mg
best non prescription ed pills ed medications online or new ed treatments
http://d-quintet.com/i/index.cgi?id=1&mode=redirect&no=494&ref_eid=33&url=https://edpills.monster ed pills for sale
best erection pills cheapest ed pills and top rated ed pills compare ed drugs
ed medications list: buying ed pills online – erectile dysfunction drug
http://levitra.icu/# Cheap Levitra online
https://sildenafil.win/# sildenafil 25 mg tablet price
http://amoxicillin.best/# buy amoxicillin 500mg uk
cipro pharmacy: buy cipro online canada – ciprofloxacin 500mg buy online
generic amoxicillin 500mg can i buy amoxicillin online amoxicillin where to get
cost of doxycycline canada: Doxycycline 100mg buy online – where can i get doxycycline online
http://azithromycin.bar/# generic zithromax 500mg india
buy cipro online without prescription Buy ciprofloxacin 500 mg online cipro pharmacy
ciprofloxacin 500mg buy online: buy ciprofloxacin over the counter – buy cipro online
cipro pharmacy ciprofloxacin generic price or ciprofloxacin generic price
https://image.google.com.qa/url?q=https://ciprofloxacin.men ciprofloxacin mail online
ciprofloxacin over the counter buy ciprofloxacin over the counter and ciprofloxacin 500 mg tablet price ciprofloxacin generic
zithromax 250 mg australia: generic zithromax online paypal – buy zithromax 1000 mg online
https://lisinopril.auction/# lisinopril 10 mg cost
doxycycline 100mg tablets cost can i buy doxycycline online or doxycycline tab india
https://cse.google.cl/url?q=https://doxycycline.forum doxycycline 110 mg
buy doxycycline capsules doxycycline capsules price in india and doxycycline otc doxycycline capsules india
buy zithromax 500mg online zithromax cost uk or can you buy zithromax over the counter in australia
http://forum.exkinoray.tv/away.php?s=http://azithromycin.bar cheap zithromax pills
generic zithromax medicine generic zithromax medicine and zithromax capsules australia zithromax 1000 mg pills
order doxycycline doxycycline buy online order doxycycline online australia
cost doxycycline: Buy doxycycline 100mg – price of doxycycline in india
generic for amoxicillin amoxicillin 250 mg price in india or amoxicillin pills 500 mg
https://toolbarqueries.google.fm/url?sa=t&url=https://amoxicillin.best amoxicillin over the counter in canada
amoxicillin 250 mg capsule order amoxicillin online no prescription and medicine amoxicillin 500 amoxicillin generic brand
http://ciprofloxacin.men/# buy cipro no rx
ciprofloxacin order online buy ciprofloxacin over the counter where can i buy cipro online
buy zithromax online australia: zithromax z-pak – zithromax over the counter canada
buy zithromax online fast shipping: zithromax z-pak – can you buy zithromax over the counter in australia
where can i buy cipro online buy ciprofloxacin tablets or buy cipro online
http://www.junix.ch/linkz.php?redir=https://ciprofloxacin.men purchase cipro
ciprofloxacin order online ciprofloxacin mail online and ciprofloxacin ciprofloxacin
http://lisinopril.auction/# lisinopril 40 mg purchase
doxycycline rx coupon doxycycline price usa or doxycycline tablets in india
https://www.google.com.ar/url?q=https://doxycycline.forum doxycycline 100 mg tablets
doxycycline 100 mg buy online purchase doxycycline online and doxycycline 100mg price 1mg doxycycline cap 40mg
buy generic zithromax online buy zithromax 1000 mg online or zithromax 500 price
https://clients1.google.sc/url?q=https://azithromycin.bar zithromax online pharmacy canada
zithromax tablets zithromax 500 mg for sale and zithromax for sale online zithromax online usa no prescription
cost of doxycycline australia: Doxycycline 100mg buy online – buy doxycycline 100 mg tablet
amoxicillin cephalexin cheap amoxicillin buy amoxicillin over the counter uk
https://doxycycline.forum/# how to get doxycycline 100mg
can we buy amoxcillin 500mg on ebay without prescription amoxicillin 800 mg price or purchase amoxicillin online without prescription
http://www.gorch-brothers.jp/modules/wordpress0/wp-ktai.php?view=redir&url=https://amoxicillin.best amoxicillin for sale online
amoxicillin 825 mg amoxicillin order online no prescription and amoxil pharmacy prescription for amoxicillin
zithromax 1000 mg pills: can you buy zithromax over the counter in canada – zithromax prescription
can you buy doxycycline over the counter australia: Buy Doxycycline for acne – doxycycline online pharmacy uk
https://mexicopharmacy.store/# mexico pharmacies prescription drugs
online drugs buy drugs online safely cheap canadian pharmacy
mexican drugstore online: mexican pharmacy – mexican pharmaceuticals online
mexican mail order pharmacies: medication from mexico pharmacy – п»їbest mexican online pharmacies
https://buydrugsonline.top/# canadian pharmacy generic viagra
mexico pharmacy reputable mexican pharmacies online or mexican mail order pharmacies
http://nwcod.com/forum/away.php?s=https://mexicopharmacy.store/ mexican pharmaceuticals online
best online pharmacies in mexico buying prescription drugs in mexico and reputable mexican pharmacies online medication from mexico pharmacy
canadian pharmacy antiobotics without prescription: order medication online – canadian drug store viagra
safe canadian online pharmacy legitimate canadian mail order pharmacy or canadian drugstore prices
https://maps.google.so/url?q=https://buydrugsonline.top discount drugs online pharmacy
overseas online pharmacy online pharmacy no prescription and viagra no prescription canadian pharmacy trust pharmacy canada
canadian pharmacy ltd: canadian pharmacies compare – canadianpharmacymeds
online pharmacy no peescription order medication online online canadian pharmacies
http://buydrugsonline.top/# best rated canadian pharmacy
list of reputable canadian pharmacies online pharmacies or pharmacy without dr prescriptions
https://www.google.dz/url?q=https://ordermedicationonline.pro canadian pharmacy world reviews
prednisone mexican pharmacy no prescription pharmacies and canada online pharmacies canadian overnight pharmacy
top online pharmacy india: world pharmacy india – reputable indian online pharmacy
reputable indian online pharmacy: best india pharmacy – pharmacy website india
http://clomid.club/# buy generic clomid without rx
http://gabapentin.life/# neurontin drug
over the counter neurontin generic gabapentin purchase neurontin online
300 mg neurontin: gabapentin best price – neurontin generic
https://gabapentin.life/# drug neurontin 200 mg
order wellbutrin online: Wellbutrin online with insurance – purchase wellbutrin online
http://claritin.icu/# buy ventolin over the counter with paypal
where buy cheap clomid without prescription: Buy Clomid Online Without Prescription – where can i buy clomid
https://paxlovid.club/# Paxlovid buy online
can you buy clomid without insurance: Buy Clomid Shipped From Canada – get cheap clomid no prescription
http://wellbutrin.rest/# wellbutrin online india
can you buy generic clomid without insurance where to buy generic clomid no prescription or can you get cheap clomid without insurance
https://images.google.hn/url?sa=t&url=https://clomid.club where to get clomid no prescription
how can i get clomid online where to buy clomid pill and how to buy generic clomid no prescription clomid order
neurontin 600 mg price neurontin cap 300mg or neurontin tablets 300mg
https://www.google.com.gt/url?q=https://gabapentin.life neurontin cost
buy neurontin online uk neurontin uk and neurontin 300 mg caps discount neurontin
paxlovid covid: buy paxlovid – Paxlovid over the counter
http://wellbutrin.rest/# wellbutrin prescription australia
buy wellbutrin online: Buy Wellbutrin XL online – wellbutrin brand name price
ventolin online nz ventolin 4mg tab or can i buy ventolin over the counter singapore
http://www.wangxiao.cn/redirect.aspx?url=https://claritin.icu/ ventolin prescription australia
ventolin uk pharmacy ventolin usa over the counter and ventolin generic price ventolin 2mg tab
paxlovid generic http://paxlovid.club/# buy paxlovid online
https://paxlovid.club/# paxlovid pharmacy
п»їpaxlovid paxlovid covid or Paxlovid buy online
http://libregraphicsworld.org/?URL=paxlovid.club paxlovid pill
paxlovid buy paxlovid cost without insurance and paxlovid pill paxlovid pill
generic clomid tablets: Buy Clomid Online Without Prescription – cost generic clomid
http://clomid.club/# how to get cheap clomid tablets
can i get clomid prices Clomiphene Citrate 50 Mg can i order generic clomid without rx
generic clomid online: Buy Clomid Online Without Prescription – how can i get clomid tablets
http://clomid.club/# clomid prices
where can i get generic clomid without rx Buy Clomid Shipped From Canada generic clomid without a prescription
paxlovid pharmacy: paxlovid price – paxlovid for sale
http://paxlovid.club/# paxlovid price
can you get generic clomid without dr prescription: Buy Clomid Online – where to get cheap clomid without a prescription
how to get clomid price: cost of cheap clomid – can i order clomid tablets
https://clomid.club/# get generic clomid tablets
where can i get clomid without rx Buy Clomid Online Without Prescription can i purchase clomid without prescription
http://gabapentin.life/# neurontin cost uk
where to buy generic clomid without rx can i order generic clomid for sale or can you buy cheap clomid pill
http://www.iheartmyteacher.org/proxy.php?link=https://clomid.club where to buy cheap clomid no prescription
how to buy generic clomid for sale where can i buy generic clomid without dr prescription and where to buy clomid no prescription how can i get cheap clomid without dr prescription
where can i buy cheap clomid without insurance: Clomiphene Citrate 50 Mg – can i buy cheap clomid price
http://clomid.club/# how can i get cheap clomid online
where buy clomid online clomid best price where can i buy generic clomid without a prescription
get generic clomid without prescription: how to get cheap clomid price – can i buy cheap clomid without prescription
https://clomid.club/# generic clomid
can i order generic clomid without rx [url=https://clomid.club/#]can you buy generic clomid pills[/url] get generic clomid tablets
where to get cheap clomid price: Buy Clomid Online – can you buy generic clomid without a prescription
http://clomid.club/# where can i buy clomid for sale
can you get generic clomid without insurance Buy Clomid Online Without Prescription buy generic clomid pill
neurontin 500 mg medicine neurontin 300 mg or neurontin 100mg cost
http://atoo.su/redirect.php?url=http://gabapentin.life neurontin prescription cost
neurontin cap 300mg price neurontin 300 mg pill and neurontin cost in singapore neurontin 300 mg pill
order generic clomid without rx: Buy Clomid Online – where can i get cheap clomid without prescription
http://clomid.club/# where to buy cheap clomid prices
where to buy cheap clomid without dr prescription Buy Clomid Online how can i get clomid
ventolin cost canada buy ventolin inhalers online or ventolin hfa 90 mcg inhaler
http://maps.google.gp/url?q=https://claritin.icu ventolin tablets buy
=cheap+cialis]buy ventolin tablets uk albuterol ventolin and ventolin 4mg buy ventolin canada
http://paxlovid.club/# paxlovid pill
order cheap clomid pills: Buy Clomid Online Without Prescription – order generic clomid tablets
https://clomid.club/# can i purchase generic clomid pills
can i get cheap clomid without prescription clomid best price can you get generic clomid pills
wellbutrin price without insurance: buy wellbutrin – 750 mg wellbutrin
buy wellbutrin online: buy wellbutrin – best price generic wellbutrin
https://clomid.club/# how to get generic clomid without dr prescription
where can i get clomid pill: clomid best price – buy generic clomid without insurance
http://clomid.club/# generic clomid no prescription
where to buy clomid prices clomid best price where to buy generic clomid without a prescription
paxlovid india paxlovid pill or paxlovid india
https://www.google.hu/url?q=https://paxlovid.club buy paxlovid online
paxlovid india paxlovid india and paxlovid covid paxlovid covid
how to buy cheap clomid no prescription: clomid best price – clomid sale
http://clomid.club/# where to buy cheap clomid pill
how to buy cheap clomid without prescription clomid best price cost of clomid without dr prescription
where to get clomid prices: Buy Clomid Shipped From Canada – cost generic clomid without a prescription
http://clomid.club/# can i order generic clomid online
how can i get cheap clomid online cost of generic clomid without insurance can i purchase cheap clomid without insurance
can i buy clomid online: Buy Clomid Online Without Prescription – buying clomid
https://clomid.club/# can you get cheap clomid prices
how can i get cheap clomid without dr prescription where can i buy clomid without a prescription buy clomid without rx
https://paxlovid.club/# Paxlovid over the counter
cost generic clomid without a prescription can you get cheap clomid without rx or where can i buy generic clomid without dr prescription
https://maps.google.je/url?q=https://clomid.club order clomid tablets
cost clomid without insurance how to get generic clomid for sale and buying clomid without rx can i get cheap clomid without rx
can i purchase clomid now: clomid best price – buying cheap clomid online
http://clomid.club/# how to buy generic clomid without rx
buy clomid generic clomid online can you get clomid pills
90 mcg ventolin: Ventolin inhaler – ventolin 2018
ventolin medicine: Ventolin inhaler online – ventolin price in usa
https://gabapentin.life/# neurontin 400
how to get cheap clomid for sale: clomid best price – order cheap clomid without dr prescription
https://clomid.club/# how to get generic clomid without a prescription
buying generic clomid prices can i buy cheap clomid without dr prescription where can i buy clomid
how to get generic clomid online: Buy Clomid Online – buying generic clomid without dr prescription
https://clomid.club/# can i purchase generic clomid pills
can i buy cheap clomid tablets clomid best price can you buy clomid no prescription
top farmacia online: Farmacie a milano che vendono cialis senza ricetta – farmacie on line spedizione gratuita
viagra online in 2 giorni dove acquistare viagra in modo sicuro cerco viagra a buon prezzo
comprare farmaci online con ricetta: farmacia online miglior prezzo – farmacie online autorizzate elenco
farmaci senza ricetta elenco: cialis generico – top farmacia online
farmacia online senza ricetta: Avanafil farmaco – farmacia online piГ№ conveniente
comprare farmaci online con ricetta: kamagra gold – farmacie online affidabili
https://farmaciait.pro/# farmacia online
comprare farmaci online con ricetta Tadalafil prezzo farmacia online miglior prezzo
farmacia online senza ricetta: kamagra gel – migliori farmacie online 2023
viagra naturale in farmacia senza ricetta: viagra consegna in 24 ore pagamento alla consegna – kamagra senza ricetta in farmacia
farmacia online migliore: kamagra gel – farmacie online autorizzate elenco
acquistare farmaci senza ricetta: avanafil generico – comprare farmaci online con ricetta
viagra ordine telefonico: viagra online spedizione gratuita – viagra online consegna rapida
farmacie online sicure: kamagra gold – comprare farmaci online con ricetta
farmaci senza ricetta elenco avanafil spedra farmacie on line spedizione gratuita
farmacia online piГ№ conveniente farmacia online piГ№ conveniente or top farmacia online
https://www.vinteger.com/scripts/redirect.php?url=https://tadalafilit.store/ farmacia online migliore
farmacia online migliore farmacie online autorizzate elenco and п»їfarmacia online migliore comprare farmaci online con ricetta
acquistare farmaci senza ricetta farmacie on line spedizione gratuita or comprare farmaci online con ricetta
http://ewin.biz/jsonp/?url=https://kamagrait.club:: farmacie online affidabili
migliori farmacie online 2023 comprare farmaci online con ricetta and farmacia online migliori farmacie online 2023
farmacie online sicure: farmacia online – comprare farmaci online all’estero
viagra 50 mg prezzo in farmacia: esiste il viagra generico in farmacia – viagra online spedizione gratuita
migliori farmacie online 2023: farmacia online miglior prezzo – farmacia online miglior prezzo
farmacia online: farmacia online piu conveniente – migliori farmacie online 2023
top farmacia online: comprare avanafil senza ricetta – farmaci senza ricetta elenco
comprare farmaci online all’estero comprare farmaci online all’estero or farmacia online piГ№ conveniente
https://images.google.ac/url?q=https://farmaciait.pro comprare farmaci online con ricetta
acquistare farmaci senza ricetta migliori farmacie online 2023 and farmacie online affidabili farmacia online migliore
comprare farmaci online con ricetta: kamagra gel prezzo – acquisto farmaci con ricetta
farmacie online sicure cialis generico consegna 48 ore farmacia online senza ricetta
https://tadalafilit.store/# comprare farmaci online con ricetta
acquisto farmaci con ricetta: Farmacie a milano che vendono cialis senza ricetta – comprare farmaci online con ricetta
viagra acquisto in contrassegno in italia viagra naturale or viagra originale in 24 ore contrassegno
https://images.google.ci/url?sa=t&url=https://sildenafilit.bid viagra ordine telefonico
=side+effects+of+sildenafil]viagra naturale in farmacia senza ricetta viagra naturale in farmacia senza ricetta and pillole per erezioni fortissime viagra originale recensioni
acquisto farmaci con ricetta: farmacia online più conveniente – top farmacia online
farmacie on line spedizione gratuita: farmacia online miglior prezzo – top farmacia online
farmacie online affidabili: farmacia online – comprare farmaci online con ricetta
farmaci senza ricetta elenco acquistare farmaci senza ricetta or acquisto farmaci con ricetta
https://toolbarqueries.google.nl/url?sa=t&url=https://tadalafilit.store farmacia online
farmacia online senza ricetta farmacia online senza ricetta and farmacia online migliore farmacia online miglior prezzo
viagra generico prezzo piГ№ basso: viagra online siti sicuri – viagra subito
farmacia online miglior prezzo: farmacia online – acquisto farmaci con ricetta
viagra originale recensioni: viagra generico – viagra generico sandoz
http://kamagrait.club/# farmacia online
farmacie online affidabili: farmacia online miglior prezzo – farmacia online
п»їfarmacia online migliore farmacia online senza ricetta or migliori farmacie online 2023
https://www.google.co.ug/url?sa=t&url=https://kamagrait.club farmacia online
п»їfarmacia online migliore farmacia online piГ№ conveniente and acquisto farmaci con ricetta farmacie online autorizzate elenco
comprare farmaci online all’estero: Farmacie che vendono Cialis senza ricetta – farmacia online più conveniente
top farmacia online: Cialis senza ricetta – top farmacia online
farmacia online: kamagra gel – comprare farmaci online all’estero
п»їfarmacia online migliore kamagra oral jelly farmacie online sicure
viagra naturale: viagra online siti sicuri – pillole per erezione in farmacia senza ricetta
farmacia senza ricetta recensioni: viagra prezzo – pillole per erezione in farmacia senza ricetta
comprare farmaci online con ricetta: farmacia online spedizione gratuita – farmacie on line spedizione gratuita
viagra 100 mg prezzo in farmacia viagra online in 2 giorni or pillole per erezione immediata
https://images.google.com.do/url?sa=t&url=https://sildenafilit.bid pillole per erezioni fortissime
viagra pfizer 25mg prezzo viagra prezzo farmacia 2023 and viagra online in 2 giorni viagra ordine telefonico
https://kamagrait.club/# acquisto farmaci con ricetta
farmacia online migliore: kamagra gel prezzo – acquisto farmaci con ricetta
farmacie online affidabili farmacia online or farmaci senza ricetta elenco
https://www.google.td/url?q=https://tadalafilit.store farmacia online
farmacie online autorizzate elenco farmacie on line spedizione gratuita and comprare farmaci online all’estero migliori farmacie online 2023
acquisto farmaci con ricetta: farmacie online autorizzate elenco – farmacia online più conveniente
farmacia online Avanafil farmaco farmacie online affidabili
farmaci senza ricetta elenco: Tadalafil prezzo – farmacie online sicure
farmacia online migliore: kamagra oral jelly – comprare farmaci online con ricetta
http://sildenafilo.store/# comprar sildenafilo cinfa 100 mg españa
farmacias baratas online envГo gratis: kamagra gel – farmacia online madrid
https://kamagraes.site/# farmacia online barata
http://kamagraes.site/# farmacia 24h
se puede comprar sildenafil sin receta viagra generico sildenafilo precio farmacia
https://vardenafilo.icu/# farmacia 24h
https://sildenafilo.store/# sildenafilo 100mg precio farmacia
https://kamagraes.site/# farmacia online internacional
farmacia online 24 horas: Precio Levitra En Farmacia – farmacias online seguras en espaГ±a
https://sildenafilo.store/# sildenafilo 100mg precio farmacia
http://sildenafilo.store/# viagra online cerca de la coruña
farmacias online seguras en espaГ±a comprar cialis online sin receta farmacia envГos internacionales
http://sildenafilo.store/# viagra online cerca de zaragoza
https://tadalafilo.pro/# farmacia online internacional
http://kamagraes.site/# farmacia online internacional
http://sildenafilo.store/# sildenafilo cinfa 100 mg precio farmacia
farmacias baratas online envГo gratis farmacias online seguras or п»їfarmacia online
https://maps.google.com.ly/url?sa=t&url=https://farmacia.best mejores farmacias online
farmacia online internacional gran farmacia online and farmacia online internacional п»їfarmacia online
https://tadalafilo.pro/# farmacia online barata
sildenafilo 50 mg precio sin receta se puede comprar sildenafil sin receta or comprar viagra contrareembolso 48 horas
https://cse.google.com.na/url?q=https://sildenafilo.store п»їViagra online cerca de Madrid
sildenafilo cinfa 100 mg precio farmacia comprar viagra en espaГ±a amazon and viagra para hombre precio farmacias comprar viagra en espaГ±a envio urgente
farmacia online madrid Precio Cialis 20 Mg farmacias baratas online envГo gratis
farmacia online internacional farmacias online baratas or п»їfarmacia online
http://preview.oberallgaeu-ferien.de/index.shtml?seite=mobile_lis&url=kamagraes.site&id=24274 farmacia 24h
farmacia online internacional farmacia 24h and farmacias online seguras en espaГ±a farmacia online internacional
http://sildenafilo.store/# se puede comprar viagra sin receta
farmacia barata: farmacia online internacional – farmacias online baratas
http://vardenafilo.icu/# farmacia envÃos internacionales
farmacia online 24 horas farmacia 24h or farmacia online 24 horas
https://www.google.com.pk/url?q=https://tadalafilo.pro farmacia online envГo gratis
farmacia barata farmacia online madrid and farmacias baratas online envГo gratis farmacia online 24 horas
http://kamagraes.site/# farmacia online envÃo gratis
https://vardenafilo.icu/# farmacia online envÃo gratis
https://tadalafilo.pro/# farmacia 24h
farmacia envГos internacionales Levitra 20 mg precio farmacia online 24 horas
https://tadalafilo.pro/# farmacias online seguras
mejor farmacia online madrid farmacia con envГos internacionales or farmacias online seguras en espaГ±a
https://maps.google.com.ly/url?sa=t&url=https://farmacia.best farmacia con envГos internacionales
mejor farmacia online madrid farmacia online internacional and farmacia con envГos internacionales farmacia online madrid
https://vardenafilo.icu/# farmacias baratas online envÃo gratis
https://kamagraes.site/# farmacia envÃos internacionales
Эффективное теплоизоляция фасадов — удобство и экономическая выгода в домашнем доме!
Согласитесь, ваш коттедж заслуживает лучшего! Теплосбережение внешних стен – не голос решение для сбережения на отоплении, это вклад в в комфорт и долговечность вашего домовладения.
✨ Почему изоляция с специалистами?
Мастерство в своем деле: Наша бригада – квалифицированные. Мы все заботимся о всей, чтобы обеспечить вашему домовладению идеальное утепление.
Сумма термоизоляции: Мы ценим ваш финансы. Утепление фасадов за 1 кв – начиная от 1350 руб./кв.м. Это вложение капитала в ваше уютное будущее!
Энергосберегающие технологии: Забудьте о потерях тепловой энергии! Наши не только сохраняют тепловое уюта, но и дарят вашему жилищу новый уровень комфорта энергоэффективности.
Обустройте свой дом уютным и стильным!
Подробнее на https://n-dom.ru
Не предоставляйте без внимания свой недвижимость на волю случайности. Доверьтесь нашей команде и создайте тепло вместе с нашей командой!
https://sildenafilo.store/# viagra 100 mg precio en farmacias
sildenafilo 50 mg precio sin receta viagra entrega inmediata or sildenafilo 100mg precio espaГ±a
http://distributors.hrsprings.com/?URL=sildenafilo.store venta de viagra a domicilio
sildenafilo 50 mg precio sin receta comprar viagra en espaГ±a amazon and sildenafilo 100mg precio farmacia comprar viagra online en andorra
https://tadalafilo.pro/# farmacia 24h
farmacias online baratas farmacias online seguras en espaГ±a or farmacias online seguras
http://www.choicesweepstakeslinks.com/link.php?url=https://kamagraes.site farmacias online seguras
farmacia envГos internacionales farmacia online madrid and farmacia online madrid farmacia barata
farmacias baratas online envГo gratis: comprar cialis online seguro – farmacias online seguras
http://farmacia.best/# farmacias online seguras en españa
https://farmacia.best/# farmacia online barata
farmacia 24h kamagra 100mg farmacias baratas online envГo gratis
https://vardenafilo.icu/# farmacia online
farmacia online internacional farmacias baratas online envГo gratis or п»їfarmacia online
http://www.mejtoft.se/research/?page=redirect&link=http://tadalafilo.pro farmacias baratas online envГo gratis
farmacias online seguras en espaГ±a farmacias online baratas and farmacias baratas online envГo gratis farmacias online baratas
http://vardenafilo.icu/# farmacia online envÃo gratis
п»їfarmacia online farmacia online madrid or farmacia 24h
https://docs.whirlpool.eu/?brand=bk&locale=de&linkreg=https://farmacia.best mejor farmacia online madrid
farmacia barata farmacia online 24 horas and farmacia internacional barcelona mejor farmacia online madrid
https://vardenafilo.icu/# farmacia envÃos internacionales
https://tadalafilo.pro/# farmacia envГos internacionales
http://sildenafilo.store/# viagra precio 2022
farmacias baratas online envГo gratis Levitra sin receta farmacia online internacional
http://vardenafilo.icu/# farmacias online seguras
http://sildenafilo.store/# sildenafilo 100mg precio farmacia
http://vardenafilo.icu/# farmacia online
farmacias online baratas: Cialis generico – farmacia 24h
https://sildenafilo.store/# viagra para hombre precio farmacias
farmacia 24h farmacia online internacional or farmacia online envГo gratis
http://m.taijiyu.net/zhuce.aspx?return=http://kamagraes.site/ farmacia 24h
п»їfarmacia online farmacia online madrid and farmacia online 24 horas farmacia online envГo gratis
http://sildenafilo.store/# comprar viagra en españa envio urgente contrareembolso
https://vardenafilo.icu/# farmacias online seguras en espaГ±a
viagra online cerca de la coruГ±a viagra online cerca de malaga or viagra entrega inmediata
http://sc.hkex.com.hk/TuniS/sildenafilo.store sildenafilo 100mg precio espaГ±a
sildenafilo 100mg precio farmacia comprar sildenafilo cinfa 100 mg espaГ±a and viagra online cerca de toledo sildenafilo 100mg sin receta
https://tadalafilo.pro/# farmacias baratas online envÃo gratis
farmacia online internacional farmacias indias online or farmacias online seguras
https://images.google.ml/url?q=https://farmacia.best farmacias baratas online envГo gratis
farmacia 24h mejores farmacias online and gran farmacia online farmacia online internacional
farmacias online seguras en espaГ±a vardenafilo sin receta п»їfarmacia online
http://sildenafilo.store/# sildenafilo sandoz 100 mg precio
venta de viagra a domicilio: viagra generico – sildenafilo 100mg precio espaГ±a
http://sildenafilo.store/# comprar viagra online en andorra
https://vardenafilo.icu/# farmacia envÃos internacionales
http://kamagraes.site/# farmacia 24h
https://farmacia.best/# farmacia online internacional
http://sildenafilo.store/# comprar viagra online en andorra
farmacia barata: farmacia online envio gratis – farmacias online seguras en espaГ±a
https://vardenafilo.icu/# farmacia 24h
farmacia online 24 horas comprar kamagra farmacias baratas online envГo gratis
suhagra price
https://sildenafilo.store/# viagra online cerca de zaragoza
farmacias baratas online envГo gratis farmacia online 24 horas or farmacias baratas online envГo gratis
https://maps.google.si/url?sa=t&url=https://kamagraes.site farmacias online baratas
farmacia online madrid farmacia 24h and farmacia barata farmacias online seguras
http://kamagraes.site/# farmacia barata
farmacia online envГo gratis murcia farmacia online canarias or farmacia online barata
https://toolbarqueries.google.co.bw/url?q=https://farmacia.best farmacia online madrid
farmacias indias online farmacia online madrid and farmacia con envГos internacionales farmacias online seguras
farmacia 24h farmacia 24h or farmacias online baratas
http://clients1.google.com.ua/url?sa=i&url=https://tadalafilo.pro farmacia online barata
farmacia envГos internacionales farmacias online baratas and farmacias online seguras en espaГ±a farmacias online baratas
https://vardenafilo.icu/# farmacia online barata
http://viagrasansordonnance.store/# Viagra vente libre pays
https://cialissansordonnance.pro/# Pharmacies en ligne certifiées
http://levitrafr.life/# Pharmacies en ligne certifiées
Viagra homme prix en pharmacie sans ordonnance Meilleur Viagra sans ordonnance 24h Viagra homme sans prescription
viagra 10 mg
http://pharmacieenligne.guru/# pharmacie en ligne
Pharmacie en ligne sans ordonnance: levitra generique prix en pharmacie – pharmacie ouverte
farmacia online 24 horas: Precio Levitra En Farmacia – farmacia online 24 horas
https://levitrafr.life/# acheter medicament a l etranger sans ordonnance
http://pharmacieenligne.guru/# pharmacie ouverte
Pharmacie en ligne fiable Levitra pharmacie en ligne Pharmacie en ligne pas cher
http://cialissansordonnance.pro/# Pharmacie en ligne fiable
https://pharmacieenligne.guru/# Pharmacie en ligne sans ordonnance
Viagra sans ordonnance livraison 48h: Acheter du Viagra sans ordonnance – Viagra femme sans ordonnance 24h
https://kamagrafr.icu/# Pharmacie en ligne sans ordonnance
Pharmacie en ligne pas cher Pharmacie en ligne sans ordonnance or pharmacie ouverte
http://etarp.com/cart/view.php?returnURL=http://kamagrafr.icu/ Pharmacie en ligne sans ordonnance
Pharmacie en ligne pas cher acheter mГ©dicaments Г l’Г©tranger and acheter medicament a l etranger sans ordonnance pharmacie ouverte
farmacia online barata: Cialis sin receta – farmacia online madrid
Viagra 100mg prix Viagra homme sans ordonnance belgique or Viagra vente libre allemagne
https://maps.google.tk/url?q=https://viagrasansordonnance.store Viagra pas cher livraison rapide france
Viagra pas cher livraison rapide france Viagra 100 mg sans ordonnance and Viagra pas cher paris Viagra homme prix en pharmacie sans ordonnance
https://levitrafr.life/# Acheter médicaments sans ordonnance sur internet
http://cialissansordonnance.pro/# acheter médicaments à l’étranger
Acheter mГ©dicaments sans ordonnance sur internet acheter kamagra site fiable Pharmacie en ligne France
http://levitrafr.life/# acheter médicaments à l’étranger
п»їpharmacie en ligne acheter medicament a l etranger sans ordonnance or Acheter mГ©dicaments sans ordonnance sur internet
https://maps.google.mw/url?q=https://pharmacieenligne.guru pharmacie ouverte 24/24
Pharmacie en ligne fiable Pharmacie en ligne sans ordonnance and pharmacie ouverte 24/24 pharmacie ouverte
http://levitrafr.life/# Pharmacies en ligne certifiées
farmacia online 24 horas: comprar cialis online seguro – farmacias baratas online envГo gratis
Viagra pas cher livraison rapide france: Viagra generique en pharmacie – Viagra 100 mg sans ordonnance
https://pharmacieenligne.guru/# Pharmacie en ligne France
pharmacie ouverte Acheter mГ©dicaments sans ordonnance sur internet or Pharmacie en ligne pas cher
https://maps.google.com.do/url?q=https://cialissansordonnance.pro Pharmacie en ligne livraison gratuite
Pharmacie en ligne pas cher Pharmacie en ligne sans ordonnance and Pharmacie en ligne fiable Pharmacie en ligne sans ordonnance
https://viagrasansordonnance.store/# Meilleur Viagra sans ordonnance 24h
http://viagrasansordonnance.store/# Sildenafil teva 100 mg sans ordonnance
https://levitrafr.life/# Pharmacie en ligne fiable
Pharmacie en ligne livraison 24h kamagra gel Pharmacie en ligne livraison gratuite
http://levitrafr.life/# Pharmacie en ligne France
farmacia online barata: kamagra – farmacia online barata
Viagra gГ©nГ©rique sans ordonnance en pharmacie: Viagra sans ordonnance 24h – Viagra femme sans ordonnance 24h
https://viagrasansordonnance.store/# Viagra sans ordonnance livraison 24h
https://levitrafr.life/# Pharmacie en ligne France
internet apotheke: potenzmittel rezeptfrei – versandapotheke
https://apotheke.company/# online apotheke deutschland
Wo kann man Viagra kaufen rezeptfrei viagra bestellen Viagra online bestellen Schweiz
online apotheke günstig: potenzmittel apotheke – online apotheke deutschland
https://kamagrakaufen.top/# online apotheke versandkostenfrei
online apotheke versandkostenfrei: versandapotheke deutschland – versandapotheke versandkostenfrei
https://kamagrakaufen.top/# versandapotheke
http://potenzmittel.men/# п»їonline apotheke
versandapotheke deutschland: Potenzmittel für Männer – günstige online apotheke
https://apotheke.company/# online apotheke versandkostenfrei
https://viagrakaufen.store/# Viagra Tabletten
online-apotheken: kamagra kaufen – online apotheke
http://viagrakaufen.store/# Viagra kaufen günstig Deutschland
Viagra kaufen gГјnstig viagra tabletten Viagra rezeptfreie Schweiz bestellen
versandapotheke: apotheke online versandkostenfrei – versandapotheke deutschland
http://cialiskaufen.pro/# online apotheke
versandapotheke: cialis preise – internet apotheke
http://apotheke.company/# online-apotheken
online apotheke versandkostenfrei versandapotheke versandkostenfrei or online apotheke gГјnstig
https://connectathon-results.ihe-europe.net/open_is_url.php?url=https://apotheke.company online apotheke preisvergleich
versandapotheke versandkostenfrei online apotheke gГјnstig and online apotheke versandkostenfrei versandapotheke
versandapotheke versandapotheke versandkostenfrei or online-apotheken
http://www.google.nl/url?sa=t&url=https://cialiskaufen.pro versandapotheke deutschland
online apotheke gГјnstig online apotheke deutschland and gГјnstige online apotheke gГјnstige online apotheke
online-apotheken: online apotheke – online apotheke versandkostenfrei
http://cialiskaufen.pro/# online apotheke versandkostenfrei
versandapotheke: potenzmittel cialis – versandapotheke deutschland
https://potenzmittel.men/# online apotheke deutschland
https://viagrakaufen.store/# Viagra kaufen ohne Rezept legal
online apotheke versandkostenfrei: potenzmittel apotheke – online-apotheken
https://cialiskaufen.pro/# online-apotheken
online apotheke versandkostenfrei: kamagra oral jelly kaufen – online-apotheken
http://kamagrakaufen.top/# versandapotheke deutschland
gГјnstige online apotheke kamagra jelly kaufen deutschland versandapotheke deutschland
https://viagrakaufen.store/# п»їViagra kaufen
online apotheke versandkostenfrei: günstige online apotheke – online apotheke versandkostenfrei
http://apotheke.company/# online apotheke günstig
п»їonline apotheke versandapotheke deutschland or gГјnstige online apotheke
https://www.google.nu/url?q=https://kamagrakaufen.top online apotheke gГјnstig
online apotheke versandkostenfrei online apotheke versandkostenfrei and online apotheke deutschland versandapotheke
versandapotheke versandkostenfrei: online apotheke – günstige online apotheke
https://kamagrakaufen.top/# versandapotheke deutschland
Sildenafil Generika 100mg: viagra generika – Wo kann man Viagra kaufen rezeptfrei
https://viagrakaufen.store/# Viagra rezeptfreie bestellen
Viagra online kaufen legal Viagra Generika 100mg rezeptfrei or Viagra Alternative rezeptfrei
https://images.google.com.jm/url?sa=t&url=https://viagrakaufen.store Viagra Generika online kaufen ohne Rezept
Viagra kaufen ohne Rezept legal Viagra kaufen gГјnstig Deutschland and Viagra online kaufen legal in Deutschland Viagra kaufen gГјnstig
http://potenzmittel.men/# online apotheke gГјnstig
versandapotheke: kamagra oral jelly – online apotheke
http://kamagrakaufen.top/# versandapotheke
versandapotheke deutschland: potenzmittel männer – versandapotheke
http://kamagrakaufen.top/# online apotheke versandkostenfrei
online apotheke gГјnstig kamagra oral jelly kaufen online apotheke gГјnstig
versandapotheke: cialis kaufen – versandapotheke
https://apotheke.company/# online apotheke
http://kamagrakaufen.top/# versandapotheke deutschland
online-apotheken: kamagra jelly kaufen deutschland – online apotheke
https://cialiskaufen.pro/# online apotheke deutschland
versandapotheke versandkostenfrei: versandapotheke versandkostenfrei – online apotheke
http://kamagrakaufen.top/# online apotheke günstig
online apotheke preisvergleich: Online Apotheke Deutschland – gГјnstige online apotheke
versandapotheke online-apotheken or internet apotheke
https://maps.google.ad/url?q=https://apotheke.company п»їonline apotheke
versandapotheke versandkostenfrei п»їonline apotheke and online apotheke preisvergleich п»їonline apotheke
versandapotheke versandkostenfrei: cialis rezeptfreie kaufen – online apotheke versandkostenfrei
https://potenzmittel.men/# online apotheke deutschland
versandapotheke deutschland п»їonline apotheke or online apotheke deutschland
https://clients1.google.co.ck/url?sa=t&url=https://cialiskaufen.pro п»їonline apotheke
online apotheke gГјnstig online apotheke preisvergleich and online-apotheken online apotheke versandkostenfrei
günstige online apotheke: kamagra oral jelly – versandapotheke versandkostenfrei
https://apotheke.company/# online-apotheken
http://viagrakaufen.store/# Sildenafil 100mg online bestellen
online-apotheken cialis generika online apotheke deutschland
online-apotheken: kamagra jelly kaufen – online apotheke versandkostenfrei
http://viagrakaufen.store/# Viagra kaufen Apotheke Preis
versandapotheke deutschland: online-apotheken – online apotheke deutschland
https://cialiskaufen.pro/# versandapotheke
online apotheke gГјnstig versandapotheke or п»їonline apotheke
http://images.google.com.gi/url?q=http://kamagrakaufen.top versandapotheke deutschland
п»їonline apotheke online apotheke deutschland and online apotheke versandkostenfrei online apotheke deutschland
https://apotheke.company/# online apotheke deutschland
internet apotheke: kamagra tabletten – online apotheke versandkostenfrei
https://viagrakaufen.store/# Viagra Generika online kaufen ohne Rezept
internet apotheke: versandapotheke – online apotheke
https://potenzmittel.men/# online apotheke versandkostenfrei
Viagra Г–sterreich rezeptfrei Apotheke Viagra kaufen gГјnstig or Sildenafil 100mg online bestellen
https://www.google.com.sg/url?q=https://viagrakaufen.store Viagra kaufen ohne Rezept Schweiz
Viagra Generika kaufen Deutschland Viagra online kaufen legal Г–sterreich and Viagra Г–sterreich rezeptfrei Apotheke Viagra kaufen ohne Rezept legal
versandapotheke: cialis kaufen – versandapotheke deutschland
http://kamagrakaufen.top/# online apotheke
best online pharmacies in mexico buying prescription drugs in mexico online buying prescription drugs in mexico online
Эффективное теплосбережение наружных стен — удобство и экономичность в приватном жилище!
Согласитесь, ваш жилище заслуживает лучшего! Утепление внешних стен – не просто решение для сбережения на тепле, это вклад в удобство и долговечность вашего недвижимости.
✨ Почему утепление с нами-мастерами?
Опыт: Наши мастера – квалифицированные специалисты. Мы все заботимся о каждой отдельной, чтобы обеспечить вашему дому идеальное термоизоляция.
Затраты теплосбережения: Мы все ценим ваш финансы. Услуги по утеплению стен снаружи стоимость работ – начиная с 1350 руб./кв.м. Это вложение капитала в ваше удобное будущее!
Энергосбережение: Забудьте о потерях тепловой энергии! Наша технология не только сохраняют тепловую энергию, но и дарят вашему домовладению новый стандарт энергоэффективности.
Преобразуйте свой домовладение комфортабельным и стильным и привлекательным!
Подробнее на http://www.stroystandart-kirov.ru
Не оставляйте свой жилище на волю случая. Доверьтесь мастерам и создайте тепло вместе с нами-профессионалами!
mexico drug stores pharmacies buying prescription drugs in mexico mexico pharmacies prescription drugs
mexican online pharmacies prescription drugs mexican drugstore online pharmacies in mexico that ship to usa
buying prescription drugs in mexico online pharmacies in mexico that ship to usa reputable mexican pharmacies online
http://mexicanpharmacy.cheap/# medication from mexico pharmacy
best online pharmacies in mexico best online pharmacies in mexico best mexican online pharmacies
http://mexicanpharmacy.cheap/# mexican drugstore online
buying prescription drugs in mexico online reputable mexican pharmacies online reputable mexican pharmacies online
medicine in mexico pharmacies п»їbest mexican online pharmacies mexican pharmaceuticals online
mexican online pharmacies prescription drugs mexican border pharmacies shipping to usa best online pharmacies in mexico
mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa buying prescription drugs in mexico
buying prescription drugs in mexico online mexican mail order pharmacies or mexico pharmacies prescription drugs
https://www.google.com.fj/url?q=https://mexicanpharmacy.cheap pharmacies in mexico that ship to usa
mexico pharmacies prescription drugs п»їbest mexican online pharmacies and medicine in mexico pharmacies mexico pharmacies prescription drugs
buying from online mexican pharmacy purple pharmacy mexico price list or mexico pharmacies prescription drugs
http://talewiki.com/cushion.php?https://mexicanpharmacy.cheap mexican mail order pharmacies
best online pharmacies in mexico mexican mail order pharmacies and mexican drugstore online buying prescription drugs in mexico online
http://mexicanpharmacy.cheap/# purple pharmacy mexico price list
https://mexicanpharmacy.cheap/# pharmacies in mexico that ship to usa
buying prescription drugs in mexico mexico drug stores pharmacies best online pharmacies in mexico
https://mexicanpharmacy.cheap/# mexican mail order pharmacies
buying prescription drugs in mexico online best online pharmacies in mexico mexico drug stores pharmacies
best mexican online pharmacies best online pharmacies in mexico medication from mexico pharmacy
mexico drug stores pharmacies mexican border pharmacies shipping to usa mexican rx online
https://mexicanpharmacy.cheap/# medication from mexico pharmacy
mexico pharmacy mexican mail order pharmacies best mexican online pharmacies
mexican drugstore online mexican rx online or mexico pharmacies prescription drugs
https://www.google.co.id/url?sa=t&url=https://mexicanpharmacy.cheap mexico drug stores pharmacies
medication from mexico pharmacy purple pharmacy mexico price list and medicine in mexico pharmacies reputable mexican pharmacies online
purple pharmacy mexico price list buying from online mexican pharmacy buying from online mexican pharmacy
mexican border pharmacies shipping to usa best online pharmacies in mexico buying from online mexican pharmacy
mexican drugstore online mexican pharmaceuticals online mexican pharmaceuticals online
mexican online pharmacies prescription drugs pharmacies in mexico that ship to usa or mexican mail order pharmacies
https://www.google.co.ls/url?q=https://mexicanpharmacy.cheap mexican drugstore online
purple pharmacy mexico price list medicine in mexico pharmacies and mexican mail order pharmacies mexican border pharmacies shipping to usa
mexico pharmacies prescription drugs best online pharmacies in mexico mexican pharmaceuticals online
mexican rx online mexican drugstore online buying prescription drugs in mexico online
purple pharmacy mexico price list mexican pharmaceuticals online mexico drug stores pharmacies
medicine in mexico pharmacies mexican mail order pharmacies mexican online pharmacies prescription drugs
mexico drug stores pharmacies mexico pharmacy or best online pharmacies in mexico
http://coolbuddy.com/newlinks/header.asp?add=http://mexicanpharmacy.cheap/ best online pharmacies in mexico
mexican rx online mexican pharmaceuticals online and pharmacies in mexico that ship to usa mexico drug stores pharmacies
legal canadian pharmacy online best canadian pharmacy online – canadian pharmacy store canadiandrugs.tech
top rated ed pills medications for ed – ed pills for sale edpills.tech
mail order pharmacy india online shopping pharmacy india п»їlegitimate online pharmacies india indiapharmacy.guru
http://canadapharmacy.guru/# canadian pharmacy online canadapharmacy.guru
https://indiapharmacy.guru/# top 10 online pharmacy in india indiapharmacy.guru
indian pharmacy online india pharmacy mail order – top 10 online pharmacy in india indiapharmacy.guru
http://edpills.tech/# erectile dysfunction drug edpills.tech
http://edpills.tech/# buying ed pills online edpills.tech
ed treatment drugs п»їerectile dysfunction medication or best ed treatment pills
https://images.google.com.au/url?q=https://edpills.tech the best ed pills
medicine erectile dysfunction ed medications online and the best ed pills best ed medication
canadian family pharmacy canadianpharmacymeds or best rated canadian pharmacy
http://www.friscowebsites.com/redirect.aspx?destination=http://canadiandrugs.tech canada drug pharmacy
canada drug pharmacy buying drugs from canada and my canadian pharmacy review real canadian pharmacy
http://edpills.tech/# buy ed pills edpills.tech
buying ed pills online generic ed pills – best ed pills online edpills.tech
mens erection pills male erection pills new ed pills edpills.tech
https://edpills.tech/# ed pills otc edpills.tech
http://edpills.tech/# best ed medication edpills.tech
https://wellbutrin.rest/# wellbutrin prices
rx clomid Clomiphene Citrate 50 Mg clomid order
http://edpills.tech/# top ed drugs edpills.tech
india pharmacy mail order india pharmacy or canadian pharmacy india
http://64.psyfactoronline.com/new/forum/away.php?s=https://indiapharmacy.pro mail order pharmacy india
reputable indian online pharmacy reputable indian pharmacies and india online pharmacy india pharmacy
reputable indian online pharmacy world pharmacy india – world pharmacy india indiapharmacy.guru
https://indiapharmacy.guru/# best online pharmacy india indiapharmacy.guru
best male enhancement pills buy ed pills online erectile dysfunction medicines edpills.tech
https://indiapharmacy.guru/# cheapest online pharmacy india indiapharmacy.guru
http://mexicanpharmacy.company/# mexico pharmacy mexicanpharmacy.company
reputable indian pharmacies indian pharmacies safe – world pharmacy india indiapharmacy.guru
https://edpills.tech/# cures for ed edpills.tech
http://canadiandrugs.tech/# global pharmacy canada canadiandrugs.tech
http://indiapharmacy.guru/# legitimate online pharmacies india indiapharmacy.guru
indian pharmacy paypal buy medicines online in india or indian pharmacy
https://www.tjarksa.com/ext.php?ref=http://indiapharmacy.guru indian pharmacies safe
reputable indian online pharmacy world pharmacy india and pharmacy website india buy medicines online in india
https://indiapharmacy.guru/# top 10 online pharmacy in india indiapharmacy.guru
reputable indian online pharmacy cheapest online pharmacy india – online shopping pharmacy india indiapharmacy.guru
reputable indian pharmacies india pharmacy mail order cheapest online pharmacy india indiapharmacy.guru
http://edpills.tech/# treatment of ed edpills.tech
http://edpills.tech/# erectile dysfunction medicines edpills.tech
best canadian pharmacy online canadian discount pharmacy – canadadrugpharmacy com canadiandrugs.tech
ed treatments ed pills otc or treatment for ed
https://www.google.co.id/url?sa=t&url=https://edpills.tech best otc ed pills
erection pills that work ed drugs list and best ed pill online ed pills
https://edpills.tech/# drugs for ed edpills.tech
canadian pharmacy online canada pharmacy online or global pharmacy canada
http://pixelpiraten.org/url?q=http://canadiandrugs.tech canadian pharmacy king
cheap canadian pharmacy canadian pharmacy mall and canada rx pharmacy adderall canadian pharmacy
http://canadiandrugs.tech/# canada pharmacy online legit canadiandrugs.tech
https://canadiandrugs.tech/# my canadian pharmacy reviews canadiandrugs.tech
canadian pharmacy 24 buying drugs from canada best canadian pharmacy to buy from canadiandrugs.tech
buy prescription drugs from india pharmacy website india or pharmacy website india
http://www.downcheck.tulihost.com/indiapharmacy.pro pharmacy website india
online pharmacy india п»їlegitimate online pharmacies india and top 10 online pharmacy in india п»їlegitimate online pharmacies india
https://indiapharmacy.guru/# indian pharmacies safe indiapharmacy.guru
best canadian pharmacy canadian mail order pharmacy – canadian pharmacy online canadiandrugs.tech
https://indiapharmacy.guru/# indianpharmacy com indiapharmacy.guru
http://indiapharmacy.guru/# top online pharmacy india indiapharmacy.guru
http://canadiandrugs.tech/# canadadrugpharmacy com canadiandrugs.tech
world pharmacy india best india pharmacy – india online pharmacy indiapharmacy.guru
п»їlegitimate online pharmacies india reputable indian pharmacies or india pharmacy mail order
http://islamcenter.ru/go.php?url=http://indiapharmacy.guru top online pharmacy india
indian pharmacies safe reputable indian pharmacies and Online medicine home delivery top 10 online pharmacy in india
http://indiapharmacy.guru/# indian pharmacy paypal indiapharmacy.guru
new ed drugs over the counter erectile dysfunction pills medicine for erectile edpills.tech
https://indiapharmacy.guru/# world pharmacy india indiapharmacy.guru
https://edpills.tech/# best pills for ed edpills.tech
india pharmacy mail order indian pharmacy – india pharmacy mail order indiapharmacy.guru
http://canadiandrugs.tech/# canadian pharmacy in canada canadiandrugs.tech
https://mexicanpharmacy.company/# best online pharmacies in mexico mexicanpharmacy.company
https://indiapharmacy.guru/# best india pharmacy indiapharmacy.guru
safe online pharmacies in canada canadian pharmacy king reviews or adderall canadian pharmacy
http://www.gamer.ru/runaway?href=http://canadiandrugs.tech legit canadian pharmacy
canadian pharmacy 365 canadian pharmacies that deliver to the us and cross border pharmacy canada northwest canadian pharmacy
http://canadiandrugs.tech/# the canadian pharmacy canadiandrugs.tech
top online pharmacy india indianpharmacy com – indian pharmacies safe indiapharmacy.guru
online pharmacy india india pharmacy best india pharmacy indiapharmacy.guru
paxlovid pill: paxlovid cost without insurance – buy paxlovid online
prednisone 10mg tablets: prednisone capsules – buying prednisone
https://amoxil.icu/# amoxicillin azithromycin
where to get clomid price: clomid generic – how to get generic clomid pill
price for amoxicillin 875 mg where to buy amoxicillin 500mg without prescription price for amoxicillin 875 mg
purchase amoxicillin online without prescription: amoxicillin medicine over the counter – amoxicillin 500 mg brand name
http://prednisone.bid/# prednisone 4mg tab
buy amoxicillin over the counter uk amoxicillin 500 mg amoxicillin 500mg capsules price
prednisone 10mg online: 20mg prednisone – prednisolone prednisone
https://ciprofloxacin.life/# buy cipro online
prednisone 20 mg without prescription: prednisone where can i buy – prednisone cream rx
ciprofloxacin order online: purchase cipro – cipro ciprofloxacin
can i buy amoxicillin over the counter in australia: where can i buy amoxicillin over the counter uk – amoxicillin 500mg price in canada
http://amoxil.icu/# buy amoxicillin online cheap
prednisone 20 tablet: where to buy prednisone in canada – prednisone buy online nz
where can i buy prednisone buy 40 mg prednisone prednisone in mexico
ciprofloxacin order online buy generic ciprofloxacin or buy generic ciprofloxacin
https://www.google.hr/url?q=https://ciprofloxacin.life cipro online no prescription in the usa
ciprofloxacin mail online buy cipro online without prescription and cipro ciprofloxacin cipro for sale
buy clomid without prescription: can you get generic clomid tablets – cost of generic clomid
http://amoxil.icu/# amoxicillin 500mg pill
paxlovid generic paxlovid price paxlovid generic
where can i get generic clomid without a prescription: cost clomid without rx – order clomid pills
prednisone daily use buy prednisone online without a script or over the counter prednisone cheap
http://www.newhopebible.net/System/Login.asp?id=49429&Referer=http://prednisone.bid buy prednisone online fast shipping
20 mg prednisone buy prednisone canada and prednisone 20 mg purchase prednisolone prednisone
where can i buy cipro online: buy cipro – ciprofloxacin generic price
ciprofloxacin mail online: buy cipro – ciprofloxacin
http://amoxil.icu/# amoxicillin 500 mg without a prescription
can i order clomid without prescription: can you get cheap clomid no prescription – how can i get cheap clomid without prescription
over the counter prednisone pills: prednisone cost us – prednisone 5 mg cheapest
https://ciprofloxacin.life/# buy cipro online without prescription
п»їpaxlovid paxlovid india buy paxlovid online
can i buy cheap clomid: cost of generic clomid pill – where can i get generic clomid without insurance
prednisone 50 mg tablet canada: 50mg prednisone tablet – prednisone price south africa
http://clomid.site/# clomid brand name
buy ciprofloxacin cipro 500mg best prices where can i buy cipro online
order prednisone 10 mg tablet: prednisone 10 mg brand name – cheapest prednisone no prescription
amoxicillin for sale where can you buy amoxicillin over the counter or azithromycin amoxicillin
https://images.google.bg/url?sa=t&url=https://amoxil.icu generic amoxicillin over the counter
amoxicillin 250 mg price in india buy amoxicillin 500mg usa and amoxicillin price without insurance buying amoxicillin online
paxlovid buy: paxlovid pill – paxlovid
Paxlovid buy online paxlovid buy or paxlovid covid
http://www.flugzeugmarkt.eu/url?q=https://paxlovid.win paxlovid pharmacy
paxlovid cost without insurance paxlovid cost without insurance and buy paxlovid online Paxlovid over the counter
paxlovid generic: paxlovid india – paxlovid generic
buy paxlovid online paxlovid pharmacy п»їpaxlovid
amoxicillin from canada: amoxicillin 500mg cost – amoxicillin 500 mg tablet price
amoxacillian without a percription: buying amoxicillin in mexico – amoxicillin generic brand
https://paxlovid.win/# Paxlovid over the counter
cialis discount price
paxlovid pill: Paxlovid buy online – Paxlovid over the counter
ciprofloxacin mail online buy cipro online canada or buy cipro online without prescription
https://www.fcviktoria.cz/media_show.asp?id=2924&id_clanek=2467&media=0&type=1&url=http://ciprofloxacin.life cipro pharmacy
ciprofloxacin buy ciprofloxacin and cipro online no prescription in the usa cipro pharmacy
how can i get cheap clomid without a prescription: can i get generic clomid without insurance – where buy generic clomid pill
https://clomid.site/# can i get clomid pills
how to get cheap clomid without a prescription can i order generic clomid without a prescription where to buy cheap clomid without dr prescription
amoxicillin 500mg cost buying amoxicillin online cost of amoxicillin 875 mg
prednisone tablets canada 5mg prednisone or prednisone for sale in canada
http://www.google.bt/url?q=https://prednisone.bid can i buy prednisone online in uk
prednisone 10 mg tablet cost prednisone uk price and prednisone 4mg 1 mg prednisone cost
https://prednisone.bid/# can you buy prednisone online uk
generic prednisone for sale can you buy prednisone in canada prednisone canada prescription
amoxicillin 875 125 mg tab: buy amoxicillin online with paypal – amoxicillin 500mg over the counter
can i buy prednisone online without a prescription: prednisone pills 10 mg – how to get prednisone tablets
https://paxlovid.win/# Paxlovid over the counter
can you buy amoxicillin over the counter canada where can i get amoxicillin amoxicillin buy online canada
amoxicillin 775 mg amoxicillin 500mg without prescription amoxicillin cost australia
amoxicillin over the counter in canada: buy amoxicillin over the counter uk – buy amoxicillin 500mg uk
http://clomid.site/# cost of clomid for sale
buy cipro cheap: ciprofloxacin 500 mg tablet price – purchase cipro
I’m really impressed with your writing skills and also with the layout on your weblog. Is this a paid theme or did you customize it yourself? Either way keep up the excellent quality writing, it is rare to see a nice blog like this one these days.
http://ciprofloxacin.life/# buy ciprofloxacin over the counter
can you get clomid without a prescription can i get generic clomid without insurance – can i get cheap clomid tablets
where can i buy generic clomid without prescription: clomid tablet – where to buy generic clomid without prescription
https://amoxil.icu/# amoxicillin 500mg capsule
2.5 mg prednisone daily: where can you buy prednisone – online order prednisone 10mg
http://amoxil.icu/# amoxicillin 250 mg capsule
Abortion pills online: buy cytotec pills – buy cytotec over the counter
https://cytotec.icu/# cytotec online
doxycycline monohydrate: where to purchase doxycycline – doxycycline order online
buy cytotec in usa: cytotec online – buy cytotec in usa
https://lisinoprilbestprice.store/# lisinopril 30 mg daily
doxycycline 100mg online: buy doxycycline cheap – buy doxycycline
doxycycline without prescription doxycycline 50 mg buy doxycycline hyclate 100mg without a rx
https://zithromaxbestprice.icu/# zithromax without prescription
who should take tamoxifen: tamoxifen breast cancer – tamoxifen menopause
https://nolvadex.fun/# nolvadex pills
buy zithromax without prescription online: buy zithromax without prescription online – zithromax z-pak
doxycycline 100mg: buy doxycycline 100mg – doxycycline
http://cytotec.icu/# buy cytotec over the counter
zithromax for sale 500 mg: zithromax cost canada – generic zithromax over the counter
https://doxycyclinebestprice.pro/# doxycycline tetracycline
buy misoprostol over the counter buy misoprostol over the counter Abortion pills online
zithromax 500mg how to get zithromax over the counter or zithromax prescription online
https://www.google.sm/url?q=https://zithromaxbestprice.icu zithromax order online uk
zithromax 500 zithromax 500 mg for sale and where to get zithromax over the counter zithromax buy
nolvadex side effects: buy tamoxifen – how to prevent hair loss while on tamoxifen
https://cytotec.icu/# Abortion pills online
buy zithromax 1000mg online: can you buy zithromax over the counter in mexico – buy zithromax online
http://cytotec.icu/# cytotec online
buy cytotec pills cytotec abortion pill buy cytotec pills
buy misoprostol over the counter: buy cytotec over the counter – Abortion pills online
https://nolvadex.fun/# buy nolvadex online
tamoxifen alternatives premenopausal: alternative to tamoxifen – what is tamoxifen used for
doxycycline 100mg online: where to get doxycycline – buy doxycycline
http://indiapharm.llc/# cheapest online pharmacy india indiapharm.llc
pharmacies in mexico that ship to usa: Purple Pharmacy online ordering – mexican rx online mexicopharm.com
https://indiapharm.llc/# top 10 pharmacies in india indiapharm.llc
indian pharmacies safe indian pharmacy to usa indian pharmacy online indiapharm.llc
mexican mail order pharmacies: Best pharmacy in Mexico – mexican pharmaceuticals online mexicopharm.com
canadian pharmacy victoza: Canada pharmacy online – canadian pharmacy king reviews canadapharm.life
best canadian online pharmacy: Canada pharmacy online – canadian discount pharmacy canadapharm.life
https://indiapharm.llc/# top 10 pharmacies in india indiapharm.llc
india pharmacy mail order: indian pharmacy to usa – п»їlegitimate online pharmacies india indiapharm.llc
http://mexicopharm.com/# mexican drugstore online mexicopharm.com
https://canadapharm.life/# canadian pharmacy scam canadapharm.life
indian pharmacies safe India Post sending medicines to USA top 10 pharmacies in india indiapharm.llc
indian pharmacy online: India pharmacy of the world – top online pharmacy india indiapharm.llc
п»їbest mexican online pharmacies: Mexico pharmacy online – reputable mexican pharmacies online mexicopharm.com
best india pharmacy: India pharmacy of the world – cheapest online pharmacy india indiapharm.llc
http://indiapharm.llc/# buy medicines online in india indiapharm.llc
indianpharmacy com: Online India pharmacy – indianpharmacy com indiapharm.llc
buying prescription drugs in mexico online: Mexico pharmacy online – mexican pharmaceuticals online mexicopharm.com
mexican pharmaceuticals online reputable mexican pharmacies online or medication from mexico pharmacy
http://www.kip-k.ru/best/sql.php?=mexicopharm.com buying from online mexican pharmacy
mexico drug stores pharmacies mexico pharmacies prescription drugs and mexico drug stores pharmacies п»їbest mexican online pharmacies
buy canadian drugs ed drugs online from canada or northwest pharmacy canada
https://toolbarqueries.google.com.bh/url?q=http://canadapharm.life canadian pharmacy world
canadian mail order pharmacy canadian pharmacy store and canada cloud pharmacy my canadian pharmacy
canadian pharmacy india: India pharmacy of the world – top 10 pharmacies in india indiapharm.llc
http://mexicopharm.com/# mexico drug stores pharmacies mexicopharm.com
pharmacy website india: indian pharmacy to usa – Online medicine order indiapharm.llc
http://canadapharm.life/# canadian pharmacy reviews canadapharm.life
indian pharmacies safe Online India pharmacy indianpharmacy com indiapharm.llc
http://canadapharm.life/# legitimate canadian pharmacy online canadapharm.life
online canadian pharmacy review: Cheapest drug prices Canada – legitimate canadian mail order pharmacy canadapharm.life
indian pharmacy online: India pharmacy of the world – indian pharmacy paypal indiapharm.llc
https://edpillsdelivery.pro/# best ed pills
cheap tadalafil tablets Tadalafil 20mg price in Canada tadalafil 20mg canada
http://sildenafildelivery.pro/# sildenafil citrate 50 mg
buy erection pills: erection pills over the counter – pills for erection
http://sildenafildelivery.pro/# how to buy sildenafil without a prescription
male ed pills cheapest ed pills erection pills viagra online
https://edpillsdelivery.pro/# ed dysfunction treatment
buy Kamagra: buy kamagra – Kamagra Oral Jelly
sildenafil citrate 100mg tablets: cheap sildenafil – sildenafil price uk
https://tadalafildelivery.pro/# tadalafil 20 mg best price
best ed pill ed pills delivery erectile dysfunction drug
http://tadalafildelivery.pro/# buy tadalafil from india
ed pills gnc: ed pills delivery – male erection pills
http://edpillsdelivery.pro/# erection pills
https://sildenafildelivery.pro/# buy online sildenafil
buy Kamagra: buy kamagra – Kamagra 100mg
sildenafil discount coupon Buy generic 100mg Sildenafil online sildenafil order
http://edpillsdelivery.pro/# cheapest ed pills online
http://edpillsdelivery.pro/# cheap erectile dysfunction pills
can i buy sildenafil over the counter in canada Buy generic 100mg Sildenafil online sildenafil 100mg cost
canada generic sildenafil: Cheapest Sildenafil online – sildenafil price 100mg
generic cialis tadalafil 20mg: Buy tadalafil online – tadalafil 30
male ed pills top erection pills or ed drugs
https://loopbaan.dezorggroep.nl/redirect.php?from=edpillsdelivery.pro best erection pills
ed medication online new treatments for ed and new ed drugs online ed medications
sildenafil coupon 100 mg sildenafil 110 mg capsule or sildenafil pills 50 mg
http://aanorthflorida.org/es/redirect.asp?url=http://sildenafildelivery.pro sildenafil 20 mg online pharmacy
sildenafil 25 mg buy online sildenafil india pharmacy and sildenafil in india online sildenafil tablets 100mg cost
Vardenafil online prescription: Generic Levitra 20mg – Levitra tablet price
http://kamagradelivery.pro/# buy kamagra online usa
Kamagra 100mg price: buy Kamagra – sildenafil oral jelly 100mg kamagra
http://levitradelivery.pro/# Buy Vardenafil 20mg online
Buy generic Levitra online Buy generic Levitra online Levitra 20 mg for sale
http://tadalafildelivery.pro/# tadalafil tablets 20 mg buy
http://edpillsdelivery.pro/# ed treatment drugs
online generic sildenafil Sildenafil price sildenafil otc canada
buy ivermectin stromectol: stromectol guru – ivermectin 1 cream generic
https://amoxil.guru/# amoxicillin 500mg
http://amoxil.guru/# amoxicillin online without prescription
https://stromectol.guru/# ivermectin 18mg
Приобретите качественные кондиционеры в известном магазине
Сделайте свой дом комфортным с нашими кондиционерами
Большой выбор кондиционеров в нашем магазине
Лучшие цены на кондиционеры только у нас
Украсьте свой интерьер с помощью наших кондиционеров
Индивидуальный подход к каждому клиенту в нашем магазине
Надежные и проверенные бренды кондиционеров в нашем ассортименте
Устраиваем быструю доставку по всей стране
Очистите воздух от пыли с помощью наших кондиционеров
Бесплатная консультация в выборе и установке кондиционеров
Осуществляем монтаж наших кондиционеров
Экономичный расход энергии с нашими кондиционерами
Регулируйте температуру в вашей квартире с нашими кондиционерами
Воспользуйтесь акцией кондиционеров в нашем магазине
Надежность наших кондиционеров от производителя
Увеличьте эффективность работы для работы с нашими кондиционерами
Индивидуальные условия для организаций при покупке кондиционеров в нашем магазине
Интуитивно понятный каталог кондиционеров на нашем сайте
Новинки в области кондиционирования в нашем магазине
Постоянно обновляемый ассортимент кондиционеров в нашем магазине
продажа кондиционеров http://www.magazin-kondicionerov.ru.
prednisone generic brand name: best prednisone – cost of prednisone 40 mg
https://clomid.auction/# can i buy clomid no prescription
can i order generic clomid pills: cheapest clomid – buying cheap clomid online
http://amoxil.guru/# order amoxicillin no prescription
order prednisone with mastercard debit: best prednisone – prednisone 5093
http://amoxil.guru/# amoxicillin 250 mg capsule
https://clomid.auction/# cost of cheap clomid no prescription
Paxlovid buy online Paxlovid buy online п»їpaxlovid
http://prednisone.auction/# medicine prednisone 10mg
buy amoxicillin online uk: cheap amoxicillin – amoxicillin over counter
http://paxlovid.guru/# Paxlovid over the counter
https://paxlovid.guru/# Paxlovid over the counter
clomid cheap: cheapest clomid – clomid prices
https://stromectol.guru/# ivermectin 200
paxlovid covid: Buy Paxlovid privately – buy paxlovid online
https://clomid.auction/# buy generic clomid prices
where can i buy oral ivermectin: cheapest stromectol – ivermectin 12
https://stromectol.guru/# stromectol ebay
http://prednisone.auction/# prednisone
Paxlovid buy online Paxlovid buy online Paxlovid over the counter
https://paxlovid.guru/# buy paxlovid online
buy amoxicillin online mexico amoxicillin 250 mg capsule or amoxicillin without rx
https://cse.google.nu/url?sa=t&url=https://amoxil.guru where can i buy amoxocillin
where can i get amoxicillin where can i buy amoxicillin over the counter uk and medicine amoxicillin 500mg amoxicillin for sale
paxlovid pill п»їpaxlovid or paxlovid pill
http://www.kgs-st-joachim.de/go.php?link=http://paxlovid.guru paxlovid pharmacy
paxlovid pill paxlovid pharmacy and п»їpaxlovid Paxlovid over the counter
ivermectin virus order stromectol or generic ivermectin for humans
http://cse.google.hn/url?sa=i&url=https://stromectol.guru ivermectin usa price
stromectol 3 mg price ivermectin 1 topical cream and ivermectin 3 mg stromectol tablets uk
buy paxlovid online: paxlovid best price – paxlovid buy
http://paxlovid.guru/# Paxlovid over the counter
http://amoxil.guru/# where can you buy amoxicillin over the counter
cost of ivermectin pill: ivermectin for sale – stromectol 3 mg tablet
where can i buy amoxocillin: can you buy amoxicillin over the counter – amoxicillin 250 mg
https://paxlovid.guru/# paxlovid pill
http://paxlovid.guru/# paxlovid generic
https://amoxil.guru/# amoxicillin azithromycin
Paxlovid over the counter: paxlovid india – buy paxlovid online
http://stromectol.guru/# ivermectin lotion cost
https://furosemide.pro/# lasix furosemide
https://finasteride.men/# buy generic propecia pill
https://lisinopril.fun/# lisinopril brand name
buy cytotec pills online cheap Misoprostol best price in pharmacy order cytotec online
lasix tablet: Buy Furosemide – lasix furosemide 40 mg
https://lisinopril.fun/# zestril 10mg price
cost of generic propecia tablets: Best place to buy propecia – cost generic propecia prices
http://azithromycin.store/# buy cheap zithromax online
http://lisinopril.fun/# lisinopril 10 mg price
generic zithromax 500mg: cheapest azithromycin – zithromax cost australia
http://finasteride.men/# generic propecia without prescription
zithromax for sale us buy zithromax 500mg online how to buy zithromax online
https://furosemide.pro/# lasix side effects
cytotec buy online usa: Misoprostol best price in pharmacy – Cytotec 200mcg price
generic prozac online
order propecia without prescription: Best place to buy propecia – order generic propecia without rx
buy cheap propecia pill: Finasteride buy online – cost propecia
https://azithromycin.store/# zithromax over the counter
lisinopril sale cheapest lisinopril lisinopril buy in canada
buy zithromax online fast shipping: buy zithromax over the counter – zithromax 500mg over the counter
lasix medication lasix uses or lasix side effects
https://images.google.com.gt/url?q=https://furosemide.pro furosemide 40 mg
buy lasix online lasix 40mg and buy furosemide online furosemide
http://furosemide.pro/# buy lasix online
https://lisinopril.fun/# lisinopril 20 mg tablets
buy generic zithromax online zithromax tablets or zithromax online
https://images.google.com.br/url?sa=t&url=https://azithromycin.store buy zithromax 1000 mg online
where can you buy zithromax generic zithromax 500mg india and how to get zithromax online how to get zithromax over the counter
https://finasteride.men/# buy propecia no prescription
cost of propecia pill order cheap propecia without prescription or buy cheap propecia
https://maps.google.com.do/url?sa=t&url=https://finasteride.men cheap propecia pill
buy propecia without a prescription cost of cheap propecia without insurance and order cheap propecia no prescription propecia without rx
zestril no prescription: buy lisinopril 10 mg tablet – buy cheap lisinopril 40mg
http://azithromycin.store/# can i buy zithromax online
cost of cheap propecia prices: Cheapest finasteride online – generic propecia pills
zithromax 500 without prescription: Azithromycin 250 buy online – zithromax for sale cheap
propecia prescription online
purchase cytotec: Buy Abortion Pills Online – buy cytotec pills online cheap
http://azithromycin.store/# zithromax 250 mg tablet price
http://lisinopril.fun/# zestril tablet
order propecia pills: Finasteride buy online – cost propecia without dr prescription
https://lisinopril.fun/# buy lisinopril
http://azithromycin.store/# zithromax capsules price
furosemida lasix dosage lasix for sale
purchase cytotec: Misoprostol best price in pharmacy – buy cytotec online
where can you buy zithromax: zithromax 250 mg pill – zithromax over the counter uk
https://furosemide.pro/# lasix uses
buy cytotec pills: cheap cytotec – buy cytotec in usa
http://lisinopril.fun/# medication lisinopril 20 mg
zithromax 500 mg: where to get zithromax – where can i purchase zithromax online
https://finasteride.men/# propecia cost
zithromax 1000 mg online can you buy zithromax over the counter in mexico or zithromax prescription online
https://cse.google.sn/url?sa=t&url=https://azithromycin.store zithromax online australia
cost of generic zithromax zithromax drug and average cost of generic zithromax zithromax without prescription
buy cytotec pills online cheap Misoprostol best price in pharmacy п»їcytotec pills online
farmacie online affidabili: cialis generico – farmaci senza ricetta elenco
http://farmaciaitalia.store/# farmacia online
https://kamagraitalia.shop/# farmacia online senza ricetta
п»їfarmacia online migliore: Farmacie a roma che vendono cialis senza ricetta – farmacie on line spedizione gratuita
farmacia online piГ№ conveniente: Avanafil farmaco – migliori farmacie online 2023
https://kamagraitalia.shop/# farmacia online
acquistare farmaci senza ricetta farmacia online spedizione gratuita farmacia online senza ricetta
farmacia online migliore: farmacia online migliore – farmacie online sicure
https://sildenafilitalia.men/# viagra acquisto in contrassegno in italia
https://farmaciaitalia.store/# farmacie on line spedizione gratuita
farmacia online senza ricetta: avanafil spedra – comprare farmaci online con ricetta
http://sildenafilitalia.men/# alternativa al viagra senza ricetta in farmacia
https://avanafilitalia.online/# farmacia online migliore
farmacia online piГ№ conveniente kamagra oral jelly farmacia online
siti sicuri per comprare viagra online: viagra prezzo farmacia – miglior sito dove acquistare viagra
viagra generico sandoz: sildenafil 100mg prezzo – kamagra senza ricetta in farmacia
https://tadalafilitalia.pro/# farmacia online migliore
viagra pfizer 25mg prezzo: viagra senza ricetta – viagra consegna in 24 ore pagamento alla consegna
mexican rx online Mexico pharmacy mexico drug stores pharmacies mexicanpharmacy.win
legitimate canadian pharmacy: Canada Pharmacy – my canadian pharmacy canadianpharmacy.pro
https://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
mexico drug stores pharmacies Mexico pharmacy reputable mexican pharmacies online mexicanpharmacy.win
https://indianpharmacy.shop/# best online pharmacy india indianpharmacy.shop
canadian prescription pharmacy
https://indianpharmacy.shop/# india pharmacy indianpharmacy.shop
medication from mexico pharmacy: mexican pharmacy online – п»їbest mexican online pharmacies mexicanpharmacy.win
rate canadian pharmacies Pharmacies in Canada that ship to the US ed meds online canada canadianpharmacy.pro
http://indianpharmacy.shop/# online pharmacy india indianpharmacy.shop
mexican drugstore online mexican pharmacy online medicine in mexico pharmacies mexicanpharmacy.win
medication from mexico pharmacy: mexico pharmacy – mexico pharmacy mexicanpharmacy.win
https://canadianpharmacy.pro/# canadian pharmacy no scripts canadianpharmacy.pro
india pharmacy Order medicine from India to USA п»їlegitimate online pharmacies india indianpharmacy.shop
legit canadian pharmacy online canadian pharmacy checker or best canadian online pharmacy
https://images.google.to/url?sa=t&url=https://canadianpharmacy.pro canadian drug pharmacy
my canadian pharmacy review legit canadian pharmacy and canadian pharmacy online canadian pharmacy cheap
https://mexicanpharmacy.win/# mexican pharmacy mexicanpharmacy.win
https://canadianpharmacy.pro/# legitimate canadian pharmacy online canadianpharmacy.pro
online prescription drugs
best online canadian pharmacy reliable canadian pharmacy canadian online pharmacy canadianpharmacy.pro
http://mexicanpharmacy.win/# buying prescription drugs in mexico mexicanpharmacy.win
http://canadianpharmacy.pro/# canadian drug stores canadianpharmacy.pro
mexican online pharmacies prescription drugs mexican drugstore online or buying from online mexican pharmacy
https://clients1.google.fi/url?q=https://mexicopharm.com п»їbest mexican online pharmacies
mexico pharmacies prescription drugs mexican online pharmacies prescription drugs and mexican online pharmacies prescription drugs mexico drug stores pharmacies
legitimate canadian pharmacies online online ed medication no prescription or canadian pharmacy price checker
https://utmagazine.ru/r?url=http://canadianpharmacy.pro pharmacy world
canadian mail order drugs canadian drugstore prices and my canadian drug store my canadian drug store
http://indianpharmacy.shop/# reputable indian pharmacies indianpharmacy.shop
http://canadianpharmacy.pro/# canada drugs online canadianpharmacy.pro
indian pharmacies safe
reputable mexican pharmacies online mexican pharmacy online buying from online mexican pharmacy mexicanpharmacy.win
canadian world pharmacy buying from canadian pharmacies or www canadianonlinepharmacy
http://www.swdh123.com/url/go.php?url=http://canadianpharmacy.pro trustworthy canadian pharmacy
pharmacy rx world canada online pharmacy canada and my canadian pharmacy rx canadian pharmacy uk delivery
http://mexicanpharmacy.win/# buying prescription drugs in mexico online mexicanpharmacy.win
Online medicine order
https://canadianpharmacy.pro/# canada drugs online reviews canadianpharmacy.pro
buying from canadian pharmacies Canada Pharmacy canadapharmacyonline com canadianpharmacy.pro
http://indianpharmacy.shop/# Online medicine home delivery indianpharmacy.shop
pharmacy website india
http://canadianpharmacy.pro/# canadian pharmacy world canadianpharmacy.pro
http://indianpharmacy.shop/# indian pharmacies safe indianpharmacy.shop
prescription drugs online without doctor
http://canadianpharmacy.pro/# canada pharmacy canadianpharmacy.pro
indian pharmacies safe buy medicines online in india or best online pharmacy india
https://maps.google.ne/url?q=https://indianpharmacy.shop reputable indian online pharmacy
indian pharmacy top online pharmacy india and india online pharmacy cheapest online pharmacy india
medication canadian pharmacy Pharmacies in Canada that ship to the US canada rx pharmacy world canadianpharmacy.pro
https://mexicanpharmacy.win/# purple pharmacy mexico price list mexicanpharmacy.win
canadian drug mart pharmacy
https://mexicanpharmacy.win/# buying prescription drugs in mexico mexicanpharmacy.win
Online medicine home delivery
mexico drug stores pharmacies buying prescription drugs in mexico online or mexico drug stores pharmacies
https://www.fahrradreisen-wanderreisen.de/redirect/Index.asp?url=http://mexicopharm.com buying prescription drugs in mexico online
mexican rx online medication from mexico pharmacy and buying from online mexican pharmacy medicine in mexico pharmacies
http://indianpharmacy.shop/# indian pharmacy indianpharmacy.shop
Online medicine home delivery indian pharmacy to usa indian pharmacies safe indianpharmacy.shop
canadian pharmacy no scripts safe canadian pharmacies or buy canadian drugs
http://www.google.ge/url?q=https://canadianpharmacy.pro canadian pharmacy meds
canadian pharmacy online reviews canadian pharmacy 1 internet online drugstore and canadian pharmacy no scripts canadian compounding pharmacy
https://indianpharmacy.shop/# india online pharmacy indianpharmacy.shop
п»їlegitimate online pharmacies india
https://mexicanpharmacy.win/# mexican online pharmacies prescription drugs mexicanpharmacy.win
https://indianpharmacy.shop/# world pharmacy india indianpharmacy.shop
safe online pharmacies online pharmacy no prescription or discount canadian pharmacy
https://cse.google.com.ai/url?sa=i&url=https://canadianpharmacy.pro canadian pharmacy prescription
canadian drugs pharmacies online canada drugs online review and canada online pharmacies canadian pharmacy androgel
indianpharmacy com indian pharmacy to usa best online pharmacy india indianpharmacy.shop
http://mexicanpharmacy.win/# buying from online mexican pharmacy mexicanpharmacy.win
best india pharmacy
https://canadianpharmacy.pro/# canada pharmacy 24h canadianpharmacy.pro
Укладка плинтуса на пол
Основные правила установки плинтуса
Подбираем оптимальный плинтус для пола
Преимущества использования плинтуса на пол
Способы укладки плинтус на пол своими руками
Полезные советы по укладке плинтуса на пол
Варианты отделки для пола
Какой плинтус выбрать для разных напольных покрытий
Нюансы монтажа плинтуса на разных поверхностях
Как выбрать цвет и материал плинтуса для пола
Монтаж плинтуса на ламинат плинтуса на ламинированный пол
Материалы для плинтуса на пол
Идеи декорирования пола с помощью плинтуса
Как закрепить плинтус на полу плинтуса для надежной фиксации
Как работают монтажные компании с плинтусами на пол
Как сделать инструмент для укладки плинтуса для монтажа плинтуса на пол
Как избежать ошибок при укладке плинтуса при монтаже плинтуса
Стоимость на плинтус для пола
Топовые производители плинтусов для пола
Интерьерные решения с помощью плинтуса
пол плинтус https://ploskye-plyntusa.ru.
https://cialissansordonnance.shop/# Pharmacie en ligne pas cher
Pharmacie en ligne fiable: pharmacie en ligne pas cher – pharmacie ouverte
pharmacie ouverte 24/24: levitrasansordonnance.pro – Pharmacie en ligne livraison 24h
http://viagrasansordonnance.pro/# Viagra pas cher livraison rapide france
Pharmacie en ligne livraison 24h PharmaDoc.pro п»їpharmacie en ligne
Pharmacie en ligne livraison gratuite: pharmacie en ligne sans ordonnance – Pharmacie en ligne France
http://cialissansordonnance.shop/# pharmacie ouverte
Acheter mГ©dicaments sans ordonnance sur internet
https://acheterkamagra.pro/# Pharmacie en ligne fiable
pharmacie ouverte 24/24 cialis prix Pharmacie en ligne France
п»їpharmacie en ligne: PharmaDoc – Pharmacie en ligne livraison rapide
Viagra gГ©nГ©rique sans ordonnance en pharmacie: Meilleur Viagra sans ordonnance 24h – Viagra sans ordonnance 24h
http://levitrasansordonnance.pro/# Pharmacie en ligne pas cher
acheter mГ©dicaments Г l’Г©tranger pharmacie en ligne pas cher Pharmacie en ligne livraison gratuite
Viagra gГ©nГ©rique pas cher livraison rapide: п»їViagra sans ordonnance 24h – Viagra pas cher inde
http://cialissansordonnance.shop/# Pharmacie en ligne livraison gratuite
Viagra femme ou trouver viagrasansordonnance.pro Meilleur Viagra sans ordonnance 24h
Viagra homme sans ordonnance belgique Viagra femme sans ordonnance 24h or SildГ©nafil 100mg pharmacie en ligne
https://www.google.ps/url?q=https://viagrasansordonnance.pro Viagra pas cher livraison rapide france
Viagra en france livraison rapide Quand une femme prend du Viagra homme and Viagra sans ordonnance 24h suisse Viagra sans ordonnance livraison 48h
Sildenafil teva 100 mg sans ordonnance: Viagra generique en pharmacie – SildГ©nafil 100mg pharmacie en ligne
https://cialissansordonnance.shop/# Pharmacie en ligne fiable
Pharmacie en ligne livraison gratuite Pharmacie en ligne livraison gratuite or acheter medicament a l etranger sans ordonnance
https://image.google.gm/url?q=j&sa=t&url=https://pharmadoc.pro Pharmacie en ligne fiable
acheter medicament a l etranger sans ordonnance Pharmacies en ligne certifiГ©es and pharmacie ouverte pharmacie ouverte 24/24
Установка кондиционера: пошаговая инструкция
mitsubishi electric кондиционер http://www.kondicionery-s-ustanovkoj.ru/.
http://levitrasansordonnance.pro/# acheter mГ©dicaments Г l’Г©tranger
Pharmacie en ligne France
Pharmacie en ligne livraison 24h: achat kamagra – Pharmacie en ligne fiable
Acheter mГ©dicaments sans ordonnance sur internet Cialis sans ordonnance 24h pharmacie ouverte 24/24
https://viagrasansordonnance.pro/# Viagra générique pas cher livraison rapide
Pharmacie en ligne France: cialis sans ordonnance – Pharmacie en ligne fiable
Pharmacie en ligne livraison 24h: cialis sans ordonnance – п»їpharmacie en ligne
acheter medicament a l etranger sans ordonnance kamagra en ligne acheter medicament a l etranger sans ordonnance
https://viagrasansordonnance.pro/# Viagra en france livraison rapide
Pharmacies en ligne certifiГ©es: achat kamagra – Pharmacie en ligne livraison gratuite
Pharmacie en ligne fiable: п»їpharmacie en ligne – п»їpharmacie en ligne
http://cialissansordonnance.shop/# Pharmacies en ligne certifiГ©es
Viagra homme prix en pharmacie sans ordonnance Viagra gГ©nГ©rique sans ordonnance en pharmacie SildГ©nafil Teva 100 mg acheter
https://pharmadoc.pro/# Acheter médicaments sans ordonnance sur internet
pharmacie ouverte 24/24 kamagra 100mg prix pharmacie ouverte
https://ivermectin.store/# ivermectin 24 mg
stromectol tablets uk: buy stromectol pills – ivermectin cream 5%
semaglutide buy australia
get cheap clomid without dr prescription how can i get generic clomid price cost cheap clomid
zithromax z-pak price without insurance: how to get zithromax over the counter – zithromax antibiotic
can i purchase prednisone without a prescription: prednisone brand name in india – prednisone 20 mg generic
http://clomiphene.icu/# can you get clomid tablets
clomid brand name: order clomid pills – how can i get cheap clomid online
https://amoxicillin.bid/# can i purchase amoxicillin online
https://clomiphene.icu/# cost of clomid now
stromectol for humans ivermectin 3 cost of stromectol medication
prednisone brand name canada: prednisone 4mg tab – 50mg prednisone tablet
http://prednisonetablets.shop/# 6 prednisone
prednisone prescription online prednisone price or prednisone 1 mg tablet
http://koukouseiquiz.net/2005/php/redirect.php?url=prednisonetablets.shop prednisone buy online nz
cost of prednisone 10mg tablets buy prednisone online no script and order prednisone 10 mg tablet prednisone pill 10 mg
can you purchase amoxicillin online order amoxicillin online cheap amoxicillin 500mg
buy prednisone canadian pharmacy: buy prednisone from india – buying prednisone on line
purchase amoxicillin online without prescription: buy amoxicillin 500mg usa – amoxicillin online canada
http://amoxicillin.bid/# amoxicillin capsule 500mg price
amoxicillin where to get: amoxicillin 500mg capsules uk – amoxicillin 500mg buy online uk
http://clomiphene.icu/# how to buy clomid price
stromectol tablets buy online ivermectin new zealand or cost of stromectol medication
http://www.city-fs.de/url?q=https://ivermectin.store cost of ivermectin 1% cream
price of ivermectin liquid ivermectin 9mg and cost of ivermectin pill stromectol buy
wegovy buy from canada
amoxicillin price without insurance: amoxicillin online purchase – amoxicillin order online
can you buy zithromax online where can i get zithromax over the counter zithromax without prescription
https://prednisonetablets.shop/# prednisone brand name india
https://azithromycin.bid/# zithromax over the counter
zithromax online pharmacy canada: where can i purchase zithromax online – cheap zithromax pills
zithromax online zithromax buy how to buy zithromax online
amoxil generic: amoxicillin brand name – buy amoxicillin 500mg usa
https://clomiphene.icu/# where can i get generic clomid now
purchase prednisone no prescription: prednisone 15 mg daily – where to buy prednisone without prescription
where can you get amoxicillin can you buy amoxicillin over the counter in canada or amoxicillin script
http://images.google.be/url?q=https://azithromycin.bid where to buy amoxicillin
buy amoxicillin can we buy amoxcillin 500mg on ebay without prescription and amoxicillin 500mg no prescription amoxicillin 500 mg capsule
http://amoxicillin.bid/# amoxicillin 500 mg cost
ivermectin syrup buy ivermectin canada or ivermectin price comparison
https://www.findmydepartment56.com/current/Department_56_Dickens_Village/Department_56_Dickens_Village_Dickens_Village_Church-sub-2.php?From=https://ivermectin.store ivermectin syrup
ivermectin goodrx ivermectin pills canada and stromectol 3 mg tablet price ivermectin syrup
where can you buy amoxicillin over the counter buy amoxicillin canada amoxicillin without a prescription
how to get cheap clomid tablets: can i get clomid no prescription – how to get clomid pills
zithromax 250 mg tablet price: buy zithromax without presc – how to get zithromax
http://prednisonetablets.shop/# prednisone 50
http://clomiphene.icu/# how can i get generic clomid
medicine prednisone 10mg: prednisone online pharmacy – cost of prednisone in canada
http://clomiphene.icu/# how to buy cheap clomid no prescription
prednisone 50 mg prices average price of prednisone or prednisone 50 mg coupon
https://www.mundijuegos.com/messages/redirect.php?url=http://prednisonetablets.shop can i buy prednisone online without prescription
prednisone 20 tablet buy prednisone online australia and prednisone uk buy 2.5 mg prednisone daily
can you buy amoxicillin over the counter in canada: medicine amoxicillin 500 – amoxicillin online purchase
cost generic clomid without a prescription can i get clomid without prescription can you get cheap clomid
where to buy amoxicillin 500mg amoxicillin 500 mg or buy amoxicillin online without prescription
https://images.google.mn/url?q=https://amoxicillin.bid where can i buy amoxocillin
price for amoxicillin 875 mg buy amoxicillin without prescription and amoxicillin order online amoxicillin 500mg price
http://indianpharm.store/# buy prescription drugs from india indianpharm.store
mexican pharmaceuticals online: Certified Pharmacy from Mexico – reputable mexican pharmacies online mexicanpharm.shop
mexican mail order pharmacies Certified Pharmacy from Mexico buying from online mexican pharmacy mexicanpharm.shop
canadian online pharmacy: Canada Pharmacy online – canada pharmacy canadianpharm.store
onlinecanadianpharmacy: Canada Pharmacy online – canada pharmacy 24h canadianpharm.store
top 10 online pharmacy in india: order medicine from india to usa – reputable indian pharmacies indianpharm.store
https://canadianpharm.store/# canadian neighbor pharmacy canadianpharm.store
medication from mexico pharmacy Online Pharmacies in Mexico mexico drug stores pharmacies mexicanpharm.shop
http://canadianpharm.store/# canadadrugpharmacy com canadianpharm.store
http://indianpharm.store/# legitimate online pharmacies india indianpharm.store
reputable indian online pharmacy: international medicine delivery from india – top 10 pharmacies in india indianpharm.store
purple pharmacy mexico price list best online pharmacies in mexico or buying prescription drugs in mexico
http://clients1.google.com.py/url?sa=t&url=https://mexicanpharm.shop:: purple pharmacy mexico price list
mexico drug stores pharmacies buying prescription drugs in mexico online and buying prescription drugs in mexico online mexican pharmaceuticals online
canadian pharmacies online Canada Pharmacy online best rated canadian pharmacy canadianpharm.store
canadian pharmacy 24 canadian pharmacies online or maple leaf pharmacy in canada
https://clients1.google.bj/url?q=https://canadianpharm.store best canadian pharmacy online
safe online pharmacies in canada reddit canadian pharmacy and reputable canadian online pharmacy my canadian pharmacy review
pharmacies in mexico that ship to usa: Online Pharmacies in Mexico – п»їbest mexican online pharmacies mexicanpharm.shop
https://canadianpharm.store/# canadian pharmacy reviews canadianpharm.store
best canadian online pharmacy: canadianpharmacyworld – canadian pharmacy ltd canadianpharm.store
Настоящий пин-ап стиль в казино
pin up aviator https://www.pinupcasinojenzolo.com.
medication from mexico pharmacy: Online Mexican pharmacy – mexican online pharmacies prescription drugs mexicanpharm.shop
canadian mail order pharmacy: Licensed Online Pharmacy – legitimate canadian mail order pharmacy canadianpharm.store
reputable mexican pharmacies online mexican pharmacy mexican pharmacy mexicanpharm.shop
http://mexicanpharm.shop/# mexico pharmacy mexicanpharm.shop
medicine in mexico pharmacies: Online Mexican pharmacy – mexican online pharmacies prescription drugs mexicanpharm.shop
world pharmacy india top 10 online pharmacy in india or top 10 pharmacies in india
https://maps.google.sc/url?sa=t&url=https://indianpharm.store pharmacy website india
india pharmacy mail order world pharmacy india and pharmacy website india Online medicine home delivery
https://mexicanpharm.shop/# pharmacies in mexico that ship to usa mexicanpharm.shop
mexican pharmaceuticals online Certified Pharmacy from Mexico mexican border pharmacies shipping to usa mexicanpharm.shop
http://indianpharm.store/# india online pharmacy indianpharm.store
vipps approved canadian online pharmacy: canadian drug pharmacy – canada rx pharmacy world canadianpharm.store
https://indianpharm.store/# pharmacy website india indianpharm.store
india online pharmacy: international medicine delivery from india – mail order pharmacy india indianpharm.store
mexican border pharmacies shipping to usa: mexican online pharmacies prescription drugs – mexico pharmacies prescription drugs mexicanpharm.shop
top 10 online pharmacy in india international medicine delivery from india best india pharmacy indianpharm.store
reputable indian online pharmacy: international medicine delivery from india – cheapest online pharmacy india indianpharm.store
https://mexicanpharm.shop/# reputable mexican pharmacies online mexicanpharm.shop
top 10 pharmacies in india: mail order pharmacy india – mail order pharmacy india indianpharm.store
canadian pharmacy world Pharmacies in Canada that ship to the US canadian pharmacy ratings canadianpharm.store
https://mexicanpharm.shop/# buying prescription drugs in mexico online mexicanpharm.shop
best online pharmacy india: buy medicines online in india – indian pharmacy indianpharm.store
mexican border pharmacies shipping to usa mexican online pharmacies prescription drugs or buying prescription drugs in mexico
https://images.google.gm/url?sa=t&url=https://mexicanpharm.shop mexican drugstore online
mexican online pharmacies prescription drugs mexican pharmaceuticals online and mexico drug stores pharmacies best online pharmacies in mexico
my canadian pharmacy best canadian online pharmacy or reputable canadian online pharmacy
http://maps.google.mv/url?sa=t&url=https://canadianpharm.store canadian online pharmacy
canadian pharmacy 24 canadian mail order pharmacy and drugs from canada canadian pharmacy 365
http://mexicanpharm.shop/# mexican online pharmacies prescription drugs mexicanpharm.shop
https://canadianpharm.store/# canadadrugpharmacy com canadianpharm.store
canadian pharmacy drugs online Licensed Online Pharmacy online canadian pharmacy canadianpharm.store
canadian pharmacy online ship to usa canadian pharmacy ed medications or canadian pharmacy 365
http://cse.google.mv/url?q=https://canadianpharm.store canadian pharmacy meds review
online pharmacy canada vipps approved canadian online pharmacy and canadian online pharmacy canadian pharmacy checker
pharmacy website india: international medicine delivery from india – indian pharmacy indianpharm.store
canadian pharmacy online: Certified Online Pharmacy Canada – canadianpharmacymeds canadianpharm.store
indian pharmacies safe: international medicine delivery from india – reputable indian online pharmacy indianpharm.store
https://mexicanpharm.shop/# buying prescription drugs in mexico mexicanpharm.shop
medicine in mexico pharmacies Online Mexican pharmacy п»їbest mexican online pharmacies mexicanpharm.shop
mexico pharmacies prescription drugs: Online Mexican pharmacy – mexican mail order pharmacies mexicanpharm.shop
indian pharmacies safe top online pharmacy india or п»їlegitimate online pharmacies india
https://www.google.co.ls/url?q=https://indianpharm.store reputable indian online pharmacy
Online medicine order cheapest online pharmacy india and Online medicine home delivery indian pharmacy paypal
http://mexicanpharm.shop/# mexico pharmacies prescription drugs mexicanpharm.shop
top 10 pharmacies in india: order medicine from india to usa – top 10 online pharmacy in india indianpharm.store
mexico drug stores pharmacies п»їbest mexican online pharmacies mexican drugstore online mexicanpharm.shop
india online pharmacy: international medicine delivery from india – top online pharmacy india indianpharm.store
https://canadianpharm.store/# recommended canadian pharmacies canadianpharm.store
http://canadadrugs.pro/# canadian internet pharmacy
canada pharmacies canada drugs online online canadian pharmacy no prescription needed
http://canadadrugs.pro/# reputable mexican pharmacies online
top rated canadian online pharmacy my mexican drugstore my mexican drugstore
canada pharmacies online prescriptions: pharmacies not requiring a prescription – pharmacy drug store online no rx
http://canadadrugs.pro/# no 1 canadian pharmacy
northeast discount pharmacy: canada prescriptions online – online ed drugs no prescription
discount prescription drugs: canadian pharmacy selling viagra – recommended canadian online pharmacies
canadian online pharmacy for viagra canadian rx prescription without a doctor’s prescription
https://canadadrugs.pro/# medicine from canada with no prescriptions
online meds without prescription: compare pharmacy prices – prescription prices comparison
http://canadadrugs.pro/# accutane mexican pharmacy
legitimate canadian pharmacies online best canadian pharmacy cialis best online pharmacy no prescription
reputable mexican pharmacies online canada rx pharmacy or best online canadian pharmacy
http://www.yu-kari-ofuna.com/feed2js/feed2js.php?src=http://canadadrugs.pro pharmacy price comparison
canadian pharcharmy canadian pharmacy in canada and canadian pharmacy ed medications aarp canadian pharmacies
most trusted canadian online pharmacy canada pharmaceuticals online canada drug
aarp recommended canadian online pharmacies: best internet pharmacies – canadian drug pharmacy
recommended canadian online pharmacies: canadian pharmacy tadalafil – canada pharmacies online pharmacy
http://canadadrugs.pro/# online drugstore service canada
canadian pharmaceuticals online best canadian pharmacies or canadian pharmacies for viagra
https://images.google.com.bn/url?q=https://canadadrugs.pro pharmacy price comparison
certified canadian pharmacy canada prescriptions online and canadian pharmacy without a prescription mexican online pharmacies
canadapharmacy com prescription online canadian pharmacies recommended
overseas pharmacy: canadian drug stores online – canadian pharmacy no prescription required
Hi,
NEW A.I App Exploits Elon Musk & ClickBank
Every 60 Seconds For $426/Paydays &
Unlimited FREE Automated Traffic!
If you are interested, write to me or follow the link: http://hornoselectricos.online/tesler/
Best Regards, Mark
http://canadadrugs.pro/# canadian drugstore prices
highest rated canadian pharmacies: canadian internet pharmacy – best mail order pharmacies
http://canadadrugs.pro/# india online pharmacy
overseas pharmacy no prescription rx medicine pharmacy price comparison
prescription pricing: canada drug pharmacy – fda approved canadian online pharmacies
http://canadadrugs.pro/# top rated online pharmacy
canadian pharmacy store: overseas pharmacies that deliver to usa – discount drugs online pharmacy
highest discount on medicines online: certified canadian international pharmacy – top mexican pharmacies
https://canadadrugs.pro/# mexican pharmacy online medications
best rated canadian pharmacy most popular canadian pharmacy or online canadian pharmaceutical companies
http://images.google.co.uz/url?q=https://canadadrugs.pro discount drugs online pharmacy
highest rated canadian pharmacies reliable mexican pharmacy and buy prescription drugs without doctor my canadian pharmacy rx reviews
canadian health pharmacy: mexican pharmacies – viagra mexican pharmacy
https://canadadrugs.pro/# canadian mail order meds
pharmacy in canada [url=https://canadadrugs.pro/#]canadian health pharmacy[/url] canada drug prices
https://canadadrugs.pro/# aarp recommended canadian pharmacies
legitimate canadian pharmacy: top rated canadian pharmacies – fda approved canadian online pharmacies
cost prescription drugs: canadian drug stores online – mexican border pharmacies
pharcharmy online no script: canadian drug companies – cheap canadian cialis
prescription drugs prices legitimate canadian pharmacies online or north canadian pharmacy
http://www.greekspider.com/target.asp?target=http://canadadrugs.pro/ canadian pharmacy pain meds
pharmacy review canadian pharmacy advair and non prescription canadian pharmacy online pharmacy without a prescription
pharmacy canada online: northeast discount pharmacy – best mexican online pharmacies
https://canadadrugs.pro/# cheap drugs online
no prescription canadian drugs: list of canadian pharmacies – mexican pharmacies online
http://canadadrugs.pro/# canadian drug store
no prescription canadian drugs canadian pharcharmy canadian pharmacies online
http://canadadrugs.pro/# canada pharmacies prescription drugs
best online drugstore canada pharmacy not requiring prescription or canadian mail order pharmacy
https://asia.google.com/url?sa=t&url=https://canadadrugs.pro canada drug prices
reliable mexican pharmacy canadian pharmacies that sell viagra and top canadian pharmacies nabp approved canadian pharmacies
http://certifiedpharmacymexico.pro/# reputable mexican pharmacies online
pills for erection: generic ed pills – best ed medications
new ed pills men’s ed pills what is the best ed pill
ed pill: top ed drugs – ed treatment pills
http://canadianinternationalpharmacy.pro/# canadian pharmacy 24 com
indian pharmacies safe: reputable indian pharmacies – reputable indian pharmacies
http://edwithoutdoctorprescription.pro/# prescription drugs without doctor approval
pet meds without vet prescription canada: canadian pharmacy com – canadian pharmacy 24h com
viagra without a doctor prescription cialis without a doctor prescription 100mg viagra without a doctor prescription
https://medicinefromindia.store/# cheapest online pharmacy india
http://edpill.cheap/# new ed pills
prescription drugs online without: viagra without a doctor prescription walmart – best ed pills non prescription
buy prescription drugs online prescription without a doctor’s prescription viagra without a doctor prescription
canada pharmacy online legit recommended canadian pharmacies or canada drugs
http://okashi-oroshi.net/modules/wordpress/wp-ktai.php?view=redir&url=http://canadianinternationalpharmacy.pro canadian pharmacy 24
reliable canadian pharmacy canadian world pharmacy and canadian king pharmacy ed drugs online from canada
best india pharmacy Online medicine order or best online pharmacy india
https://www.google.by/url?q=https://medicinefromindia.store indianpharmacy com
indian pharmacy india pharmacy and india pharmacy mail order buy medicines online in india
https://edpill.cheap/# top ed pills
Dear Sir,
Discover the future of earning through our groundbreaking AI-powered Passive Income System! This innovative solution offers you an effortless way to generate passive income by leveraging the power of Artificial Intelligence to identify and capitalize on lucrative opportunities in real-time. Whether you’re new to passive income or looking to diversify your portfolio, our system is designed to maximize returns with minimal effort on your part. Experience the simplicity of setting up, the thrill of watching your earnings grow, and the peace of mind that comes with secure, AI-driven investments. Don’t miss out on this chance to transform your financial future. Contact us now to learn more and embark on your journey to financial freedom with AI!
learn More: https://hornoselectricos.online/PayPerCallAI/
Best regards,
Bill Cooper.
mexican pharmaceuticals online mexican online pharmacies prescription drugs buying from online mexican pharmacy
online prescription for ed meds: ed pills without doctor prescription – prescription without a doctor’s prescription
https://edwithoutdoctorprescription.pro/# non prescription ed drugs
legal to buy prescription drugs from canada: reputable canadian online pharmacy – canadian neighbor pharmacy
http://edwithoutdoctorprescription.pro/# best ed pills non prescription
indian pharmacy paypal pharmacy website india or buy prescription drugs from india
http://clients1.google.ge/url?q=https://medicinefromindia.store reputable indian pharmacies
Online medicine home delivery top 10 online pharmacy in india and reputable indian pharmacies Online medicine home delivery
top erection pills best ed drugs drugs for ed
https://edpill.cheap/# cheap ed pills
Thanks for the complete information. You helped me.
viagra without a doctor prescription: generic cialis without a doctor prescription – prescription drugs canada buy online
https://edwithoutdoctorprescription.pro/# real viagra without a doctor prescription
escrow pharmacy canada canada cloud pharmacy or rate canadian pharmacies
https://community.pharos.com/external-link.jspa?url=http://canadianinternationalpharmacy.pro canadian pharmacy reviews
canadian discount pharmacy canadian 24 hour pharmacy and canada discount pharmacy canadian pharmacy world
ed meds ed dysfunction treatment best medication for ed
https://canadianinternationalpharmacy.pro/# northwest canadian pharmacy
reputable mexican pharmacies online п»їbest mexican online pharmacies or pharmacies in mexico that ship to usa
https://maps.google.sc/url?q=https://certifiedpharmacymexico.pro mexico drug stores pharmacies
mexican border pharmacies shipping to usa mexico drug stores pharmacies and purple pharmacy mexico price list mexican border pharmacies shipping to usa
indianpharmacy com best india pharmacy or п»їlegitimate online pharmacies india
https://www.google.se/url?q=https://medicinefromindia.store cheapest online pharmacy india
top online pharmacy india online shopping pharmacy india and mail order pharmacy india india online pharmacy
ed meds online without doctor prescription: cheap cialis – non prescription ed pills
top online pharmacy india best india pharmacy pharmacy website india
http://edwithoutdoctorprescription.pro/# non prescription ed pills
canadapharmacyonline com: canadian king pharmacy – cross border pharmacy canada
https://edpill.cheap/# ed pills gnc
cialis without doctor prescription cheap cialis ed meds online without doctor prescription
http://certifiedpharmacymexico.pro/# best mexican online pharmacies
reputable indian pharmacies Online medicine home delivery or indian pharmacies safe
https://cse.google.mn/url?sa=t&url=https://medicinefromindia.store top 10 online pharmacy in india
best online pharmacy india indian pharmacy and india pharmacy п»їlegitimate online pharmacies india
viagra without doctor prescription amazon cialis without a doctor prescription canada buy prescription drugs without doctor
http://edpill.cheap/# treatment of ed
reputable canadian pharmacy best canadian pharmacy or buying from canadian pharmacies
http://lonevelde.lovasok.hu/out_link.php?url=http://canadianinternationalpharmacy.pro/ canadian pharmacy online store
online canadian pharmacy canadian drug and www canadianonlinepharmacy reputable canadian pharmacy
onlinepharmaciescanada com: canada pharmacy reviews – certified canadian pharmacy
https://medicinefromindia.store/# online shopping pharmacy india
mexico drug stores pharmacies purple pharmacy mexico price list medication from mexico pharmacy
Did you know about the new AI capabilities?
Use them for your business before your competitors do.
https://www.youtube.com/watch?v=cz2A9q9PVuU
natural ed remedies: erectile dysfunction medicines – generic ed drugs
http://medicinefromindia.store/# best india pharmacy
Получи права управлять автомобилем в лучшей автошколе!
Стремись к профессиональной карьере автолюбителя с нашей автошколой!
Успей пройти обучение в самой автошколе города!
Задай тон правильного вождения с нашей автошколой!
Стремись к безупречным навыкам вождения с нашей автошколой!
Начни уверенно водить автомобиль у нас в автошколе!
Достигай независимости и свободы, получив права в автошколе!
Продемонстрируй мастерство вождения в нашей автошколе!
Открой новые возможности, получив права в автошколе!
Приведи друзей и они получат скидку на обучение в автошколе!
Стань профессиональному будущему в автомобильном мире с нашей автошколой!
новые друзья и научись водить автомобиль вместе с нашей автошколой!
Развивай свои навыки вождения вместе с опытными инструкторами нашей автошколы!
Закажи обучение в автошколе и получи бесплатный индивидуальный урок от наших инструкторов!
Стремись к надежности и безопасности на дороге вместе с нашей автошколой!
Улучши свои навыки вождения вместе с профессионалами в нашей автошколе!
Учись дорожные правила и навыки вождения в нашей автошколе!
Стремись к настоящим мастером вождения с нашей автошколой!
Накопи опыт вождения и получи права в нашей автошколе!
Покори дорогу вместе с нами – пройди обучение в автошколе!
отримати права водія https://avtoshkolaznit.kiev.ua .
http://edwithoutdoctorprescription.pro/# real viagra without a doctor prescription
best online pharmacies in mexico medication from mexico pharmacy mexico drug stores pharmacies
http://edpill.cheap/# erectile dysfunction drugs
canadian drugs online canada drugs canada drug pharmacy
buy erection pills: gnc ed pills – ed medications online
https://edpill.cheap/# best ed treatment
best india pharmacy reputable indian online pharmacy or Online medicine home delivery
https://images.google.com.kh/url?q=https://medicinefromindia.store top 10 pharmacies in india
п»їlegitimate online pharmacies india п»їlegitimate online pharmacies india and indian pharmacy online п»їlegitimate online pharmacies india
pharmacy website india: online pharmacy india – cheapest online pharmacy india
https://medicinefromindia.store/# online pharmacy india
pharmacies in mexico that ship to usa mexican border pharmacies shipping to usa buying from online mexican pharmacy
https://certifiedpharmacymexico.pro/# pharmacies in mexico that ship to usa
buying prescription drugs in mexico online mexican online pharmacies prescription drugs or best online pharmacies in mexico
https://maps.gngjd.com/url?q=https://certifiedpharmacymexico.pro mexican mail order pharmacies
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa and mexico pharmacies prescription drugs mexico drug stores pharmacies
reputable canadian pharmacy buy drugs from canada or canadian pharmacy uk delivery
https://reverb.com/onward?author_id=5021397&to=https://canadianinternationalpharmacy.pro canada discount pharmacy
canadian discount pharmacy canadian pharmacy 365 and canadian neighbor pharmacy legitimate canadian pharmacies
https://edpill.cheap/# cure ed
mexican rx online mexican rx online buying prescription drugs in mexico
india pharmacy mail order п»їlegitimate online pharmacies india or best india pharmacy
http://www.google.com.om/url?q=https://medicinefromindia.store top 10 pharmacies in india
best online pharmacy india cheapest online pharmacy india and Online medicine home delivery india pharmacy mail order
https://canadianinternationalpharmacy.pro/# legal to buy prescription drugs from canada
canadian pharmacy online reviews canadian pharmacy online reviews safe canadian pharmacy
cheapest online pharmacy india: cheapest online pharmacy india – pharmacy website india
canadian pharmacy online: canadian pharmacy ltd – best canadian online pharmacy
https://certifiedpharmacymexico.pro/# mexican pharmaceuticals online
https://medicinefromindia.store/# india online pharmacy
I am no longer certain where you’re getting your information, but good topic. I must spend a while studying much more or understanding more. Thank you for fantastic information I was on the lookout for this information for my mission.
https://canadianinternationalpharmacy.pro/# canadian pharmacy drugs online
F*ckin’ tremendous things here. I am very glad to see your post. Thanks a lot and i am looking forward to contact you. Will you kindly drop me a e-mail?
non prescription ed drugs best drug for ed erectile dysfunction pills
india pharmacy mail order mail order pharmacy india or online pharmacy india
http://ooshnovosel.ru/bitrix/redirect.php?event1=&event2=&event3=&goto=https://medicinefromindia.store/ reputable indian pharmacies
indian pharmacy paypal pharmacy website india and best online pharmacy india Online medicine home delivery
http://edwithoutdoctorprescription.pro/# viagra without a doctor prescription walmart
reputable indian online pharmacy online shopping pharmacy india buy prescription drugs from india
http://edwithoutdoctorprescription.pro/# prescription drugs canada buy online
reputable canadian online pharmacies pet meds without vet prescription canada or canadian online pharmacy
https://clients1.google.co.uz/url?q=https://canadianinternationalpharmacy.pro canada pharmacy online legit
canadian 24 hour pharmacy ed meds online canada and canadian pharmacy king the canadian pharmacy
ed meds online without prescription or membership: ed pills without doctor prescription – cialis without a doctor’s prescription
buying prescription drugs in mexico online: mexico pharmacies prescription drugs – purple pharmacy mexico price list
https://edwithoutdoctorprescription.pro/# ed meds online without doctor prescription
buy prescription drugs from canada cheap cialis without a doctor prescription prescription drugs without doctor approval
best mexican online pharmacies reputable mexican pharmacies online purple pharmacy mexico price list
mexican mail order pharmacies purple pharmacy mexico price list medicine in mexico pharmacies
buy semaglutide oversees
mexican pharmacy pharmacies in mexico that ship to usa medicine in mexico pharmacies
http://mexicanph.shop/# buying from online mexican pharmacy
purple pharmacy mexico price list buying prescription drugs in mexico online mexican mail order pharmacies
https://mexicanph.shop/# buying prescription drugs in mexico
medicine in mexico pharmacies
mexican rx online buying prescription drugs in mexico online buying from online mexican pharmacy
mexican mail order pharmacies mexico pharmacy or mexican pharmaceuticals online
http://www.eloiseplease.com/?URL=mexicanph.com mexico drug stores pharmacies
mexico pharmacies prescription drugs mexican rx online and medication from mexico pharmacy mexican border pharmacies shipping to usa
buying prescription drugs in mexico online mexico drug stores pharmacies reputable mexican pharmacies online
Уважаемые Гости!
Предоставляем вам свежее элемент в мире декора интерьера – шторы плиссе. Если вы рассчитываете к высшему качеству в всякой части вашего дома, то эти шторы превратятся прекрасным паттерном для вас.
Что делает шторы плиссе настолько же оригинальными? Они совмещают в себе в себе изящество, работоспособность и применимость. Благодаря характерной архитектуре, последним материям, шторы плиссе идеально подходятся для какого бы то ни пола, будь то зала, ложе, плитка или должностное пространство.
Закажите жалюзи плиссе – сформируйте уют и прекрасность в вашем доме!
Чем подсаживают шторы плиссе для вас? Во-первых, их поразительный бренд, который присоединяет привлекательность и элегантность вашему месту. Вы можете подобрать из разнообразных текстур, цветов и подходов, чтобы выделить индивидуальность вашего дома.
Кроме того, шторы плиссе предлагают обширный ряд функциональных возможностей. Они могут контролировать степень освещения в помещении, покрывать от солнечного света, предоставлять закрытость и формировать уютную среду в вашем доме.
Наш веб-сайт: http://tulpan-pmr.ru
Мы сами поможем вам выбрать шторы плиссе, какие замечательно подходят к для вашего внутреннего пространства!
п»їbest mexican online pharmacies purple pharmacy mexico price list mexican border pharmacies shipping to usa
https://mexicanph.com/# mexican online pharmacies prescription drugs
purple pharmacy mexico price list
mexican online pharmacies prescription drugs reputable mexican pharmacies online mexican pharmaceuticals online
buy semaglutide in mexico
pharmacies in mexico that ship to usa mexican mail order pharmacies mexican drugstore online
mexican pharmacy best online pharmacies in mexico or mexican border pharmacies shipping to usa
https://www.google.tg/url?q=https://mexicanph.com buying prescription drugs in mexico online
buying prescription drugs in mexico mexican pharmaceuticals online and medicine in mexico pharmacies mexico pharmacy
medication from mexico pharmacy mexican pharmaceuticals online purple pharmacy mexico price list
reputable mexican pharmacies online mexican pharmacy mexican online pharmacies prescription drugs
https://mexicanph.shop/# medication from mexico pharmacy
purple pharmacy mexico price list best online pharmacies in mexico medication from mexico pharmacy
mexican rx online п»їbest mexican online pharmacies or medicine in mexico pharmacies
https://anolink.com/?link=https://mexicanph.shop mexican pharmaceuticals online
pharmacies in mexico that ship to usa buying from online mexican pharmacy and mexican drugstore online medicine in mexico pharmacies
https://mexicanph.com/# medication from mexico pharmacy
medicine in mexico pharmacies
mexican drugstore online mexico drug stores pharmacies or buying prescription drugs in mexico online
http://www.google.tt/url?q=https://mexicanph.com reputable mexican pharmacies online
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa and mexico drug stores pharmacies pharmacies in mexico that ship to usa
mexican drugstore online pharmacies in mexico that ship to usa mexican border pharmacies shipping to usa
buying prescription drugs in mexico online mexico pharmacies prescription drugs п»їbest mexican online pharmacies
buying from online mexican pharmacy п»їbest mexican online pharmacies medicine in mexico pharmacies
http://mexicanph.com/# buying prescription drugs in mexico
mexico drug stores pharmacies mexican border pharmacies shipping to usa mexican drugstore online
mexico drug stores pharmacies mexican border pharmacies shipping to usa or mexico drug stores pharmacies
https://maps.google.bi/url?q=https://mexicanph.com mexican pharmaceuticals online
mexican border pharmacies shipping to usa mexico drug stores pharmacies and mexico drug stores pharmacies medicine in mexico pharmacies
mexican mail order pharmacies medicine in mexico pharmacies mexican border pharmacies shipping to usa
buying prescription drugs in mexico online pharmacies in mexico that ship to usa or best online pharmacies in mexico
https://www.google.nr/url?q=https://mexicanph.shop purple pharmacy mexico price list
medicine in mexico pharmacies buying from online mexican pharmacy and mexico pharmacy buying prescription drugs in mexico
is zithromax over the counter
reputable mexican pharmacies online buying from online mexican pharmacy medication from mexico pharmacy
https://mexicanph.com/# mexican border pharmacies shipping to usa
buying prescription drugs in mexico
mexican pharmaceuticals online reputable mexican pharmacies online mexico pharmacies prescription drugs
mexican mail order pharmacies mexico pharmacies prescription drugs reputable mexican pharmacies online
medication from mexico pharmacy mexico pharmacy mexico drug stores pharmacies
mexican drugstore online medication from mexico pharmacy or п»їbest mexican online pharmacies
http://ppp.ph/jp/bin/bbs/redirect.php?u=http://mexicanph.com medicine in mexico pharmacies
purple pharmacy mexico price list mexican rx online and mexican pharmacy mexican online pharmacies prescription drugs
mexican online pharmacies prescription drugs mexican rx online mexican border pharmacies shipping to usa
http://mexicanph.com/# mexican online pharmacies prescription drugs
buying prescription drugs in mexico reputable mexican pharmacies online mexico drug stores pharmacies
mexican rx online mexico pharmacies prescription drugs best online pharmacies in mexico
buying prescription drugs in mexico online buying prescription drugs in mexico online buying prescription drugs in mexico
pharmacies in mexico that ship to usa mexico pharmacy buying prescription drugs in mexico online
mexican online pharmacies prescription drugs mexican pharmacy mexican online pharmacies prescription drugs
mexican border pharmacies shipping to usa п»їbest mexican online pharmacies or mexico pharmacies prescription drugs
http://arinastar.ru/forum/away.php?s=https://mexicanph.shop purple pharmacy mexico price list
best online pharmacies in mexico pharmacies in mexico that ship to usa and mexico drug stores pharmacies buying from online mexican pharmacy
http://mexicanph.shop/# medicine in mexico pharmacies
medication from mexico pharmacy
mexican drugstore online mexico drug stores pharmacies mexican border pharmacies shipping to usa
mexico drug stores pharmacies best mexican online pharmacies mexican border pharmacies shipping to usa
mexican pharmaceuticals online mexican online pharmacies prescription drugs buying prescription drugs in mexico online
medication from mexico pharmacy purple pharmacy mexico price list or best online pharmacies in mexico
https://clients1.google.fi/url?q=https://mexicanph.shop buying prescription drugs in mexico online
buying prescription drugs in mexico mexico drug stores pharmacies and buying prescription drugs in mexico online mexican border pharmacies shipping to usa
pharmacies in mexico that ship to usa buying from online mexican pharmacy or buying from online mexican pharmacy
http://www.transitaire.info/cgi-bin/erawan/smartframe.cgi?http://mexicanph.com/ mexican border pharmacies shipping to usa
reputable mexican pharmacies online mexican mail order pharmacies and mexican border pharmacies shipping to usa п»їbest mexican online pharmacies
best mexican online pharmacies mexico drug stores pharmacies mexico pharmacy
buying from online mexican pharmacy [url=https://mexicanph.shop/#]mexican border pharmacies shipping to usa[/url] mexican pharmacy
mexican pharmaceuticals online buying prescription drugs in mexico online or best online pharmacies in mexico
https://cse.google.nr/url?sa=t&url=https://mexicanph.com best online pharmacies in mexico
п»їbest mexican online pharmacies pharmacies in mexico that ship to usa and buying from online mexican pharmacy buying prescription drugs in mexico
mexican mail order pharmacies pharmacies in mexico that ship to usa buying prescription drugs in mexico online
mexico pharmacies prescription drugs mexican online pharmacies prescription drugs mexican border pharmacies shipping to usa
https://mexicanph.com/# mexican drugstore online
mexican online pharmacies prescription drugs reputable mexican pharmacies online mexico drug stores pharmacies
best online pharmacies in mexico mexico pharmacies prescription drugs mexican pharmaceuticals online
medication from mexico pharmacy mexican pharmacy buying prescription drugs in mexico
pharmacies in mexico that ship to usa mexican pharmaceuticals online mexico pharmacy
mexico pharmacy medication from mexico pharmacy purple pharmacy mexico price list
https://mexicanph.com/# purple pharmacy mexico price list
mexican pharmaceuticals online
mexico drug stores pharmacies buying from online mexican pharmacy reputable mexican pharmacies online
п»їbest mexican online pharmacies reputable mexican pharmacies online buying from online mexican pharmacy
mexico pharmacy reputable mexican pharmacies online medicine in mexico pharmacies
mexican drugstore online reputable mexican pharmacies online mexican pharmacy
purple pharmacy mexico price list mexican pharmacy medicine in mexico pharmacies
mexican border pharmacies shipping to usa best mexican online pharmacies buying from online mexican pharmacy
mexico drug stores pharmacies pharmacies in mexico that ship to usa or purple pharmacy mexico price list
https://maps.google.dm/url?q=https://mexicanph.com mexican online pharmacies prescription drugs
buying prescription drugs in mexico buying from online mexican pharmacy and best online pharmacies in mexico medication from mexico pharmacy
http://mexicanph.com/# buying from online mexican pharmacy
medicine in mexico pharmacies buying from online mexican pharmacy mexican mail order pharmacies
medication from mexico pharmacy mexican drugstore online purple pharmacy mexico price list
best online pharmacies in mexico reputable mexican pharmacies online mexican online pharmacies prescription drugs
п»їbest mexican online pharmacies mexico pharmacies prescription drugs mexico pharmacy
mexico drug stores pharmacies mexico pharmacy buying from online mexican pharmacy
reputable mexican pharmacies online best online pharmacies in mexico or mexico pharmacies prescription drugs
http://images.google.ee/url?q=http://mexicanph.shop buying from online mexican pharmacy
purple pharmacy mexico price list medication from mexico pharmacy and mexican mail order pharmacies mexican rx online
http://mexicanph.shop/# best online pharmacies in mexico
mexico drug stores pharmacies
mexico pharmacy buying from online mexican pharmacy reputable mexican pharmacies online
buying from online mexican pharmacy mexico drug stores pharmacies mexico drug stores pharmacies
mexico drug stores pharmacies buying prescription drugs in mexico mexican online pharmacies prescription drugs
mexican border pharmacies shipping to usa buying prescription drugs in mexico mexican pharmacy
mexican border pharmacies shipping to usa buying prescription drugs in mexico reputable mexican pharmacies online
mexican mail order pharmacies buying prescription drugs in mexico online or best online pharmacies in mexico
https://securegpform.co.uk/1/mexicanph.shop mexican border pharmacies shipping to usa
reputable mexican pharmacies online best online pharmacies in mexico and mexico drug stores pharmacies medicine in mexico pharmacies
mexico pharmacy reputable mexican pharmacies online mexican online pharmacies prescription drugs
mexican mail order pharmacies buying prescription drugs in mexico medicine in mexico pharmacies
buying prescription drugs in mexico best online pharmacies in mexico or mexican rx online
http://www.google.com.my/url?q=https://mexicanph.com mexican pharmaceuticals online
buying prescription drugs in mexico mexico pharmacy and mexican border pharmacies shipping to usa purple pharmacy mexico price list
buying prescription drugs in mexico mexico drug stores pharmacies purple pharmacy mexico price list
mexican rx online mexican rx online mexican mail order pharmacies
https://mexicanph.com/# mexican online pharmacies prescription drugs
buying prescription drugs in mexico online mexican rx online п»їbest mexican online pharmacies
mexican border pharmacies shipping to usa best online pharmacies in mexico mexico drug stores pharmacies
mexican mail order pharmacies buying prescription drugs in mexico online п»їbest mexican online pharmacies
reputable mexican pharmacies online mexican online pharmacies prescription drugs buying prescription drugs in mexico online
mexico pharmacy mexican drugstore online mexico pharmacies prescription drugs
https://mexicanph.shop/# mexican rx online
mexican border pharmacies shipping to usa
mexican border pharmacies shipping to usa п»їbest mexican online pharmacies or best online pharmacies in mexico
https://cse.google.com.jm/url?sa=t&url=https://mexicanph.com buying prescription drugs in mexico online
reputable mexican pharmacies online medicine in mexico pharmacies and medication from mexico pharmacy mexican mail order pharmacies
п»їbest mexican online pharmacies pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa
mexico drug stores pharmacies best online pharmacies in mexico mexican mail order pharmacies
mexico drug stores pharmacies mexican rx online mexican online pharmacies prescription drugs
mexican border pharmacies shipping to usa mexico pharmacy or mexican pharmaceuticals online
http://clients1.google.co.za/url?sa=t&url=https://mexicanph.com medication from mexico pharmacy
medication from mexico pharmacy mexican pharmaceuticals online and mexican pharmaceuticals online mexico drug stores pharmacies
mexico drug stores pharmacies mexican pharmaceuticals online buying prescription drugs in mexico online
mexican mail order pharmacies mexico drug stores pharmacies buying from online mexican pharmacy
buying from online mexican pharmacy mexican online pharmacies prescription drugs mexican border pharmacies shipping to usa
mexican pharmacy medicine in mexico pharmacies buying prescription drugs in mexico online
mexican border pharmacies shipping to usa mexico pharmacies prescription drugs mexico drug stores pharmacies
mexican rx online purple pharmacy mexico price list buying prescription drugs in mexico
mexican rx online mexico drug stores pharmacies or mexican pharmacy
http://www.pro100chat.ru/go.php?url=https://mexicanph.shop buying from online mexican pharmacy
medication from mexico pharmacy mexico drug stores pharmacies and best online pharmacies in mexico п»їbest mexican online pharmacies
what is metformin used for other than diabetes
https://mexicanph.com/# medicine in mexico pharmacies
medicine in mexico pharmacies buying prescription drugs in mexico mexican online pharmacies prescription drugs
mexico pharmacies prescription drugs reputable mexican pharmacies online best mexican online pharmacies
purple pharmacy mexico price list mexican drugstore online buying prescription drugs in mexico
https://mexicanph.com/# mexican drugstore online
mexico pharmacies prescription drugs
mexican drugstore online mexico drug stores pharmacies mexico pharmacies prescription drugs
pharmacies in mexico that ship to usa medication from mexico pharmacy or mexican online pharmacies prescription drugs
https://images.google.co.ck/url?q=https://mexicanph.com mexican pharmaceuticals online
mexican drugstore online mexican online pharmacies prescription drugs and mexican mail order pharmacies buying prescription drugs in mexico
cheap cialis online canadian pharmacy explanation
canada pharmacy for viagra online canadian pharmacy
mexican mail order pharmacies medicine in mexico pharmacies purple pharmacy mexico price list
best online pharmacies in mexico mexico drug stores pharmacies medication from mexico pharmacy
http://amoxil.cheap/# amoxicillin 250 mg
can i purchase amoxicillin online buy amoxicillin online mexico amoxicillin without a prescription
buy ivermectin for humans australia: ivermectin tablet 1mg – ivermectin cost australia
https://furosemide.guru/# furosemide 100 mg
http://amoxil.cheap/# amoxicillin 500 mg purchase without prescription
https://amoxil.cheap/# can i buy amoxicillin over the counter in australia
url lisinopril hctz prescription: can i order lisinopril online – lisinopril medicine
prednisone 4mg prednisone pills 10 mg prednisone 2.5 mg
https://stromectol.fun/# buy minocycline 50 mg tablets
buy prednisone 1 mg mexico prednisone 10 mg canada how to get prednisone tablets
http://stromectol.fun/# ivermectin 0.08 oral solution
prednisone 300mg: can you buy prednisone over the counter in usa – 25 mg prednisone
https://stromectol.fun/# ivermectin 50 mg
cost of amoxicillin prescription amoxicillin tablets in india amoxicillin no prescription
http://lisinopril.top/# lisinopril brand name australia
furosemide 100mg: Buy Furosemide – furosemide 100 mg
https://furosemide.guru/# lasix online
lasix for sale Buy Furosemide lasix generic
ivermectin 1 topical cream: ivermectin 1% – ivermectin lotion price
http://furosemide.guru/# lasix generic name
https://buyprednisone.store/# prednisone 10
minocycline 100 mg tablet ivermectin pills human stromectol tablets buy online
http://buyprednisone.store/# prednisone prescription drug
buy prednisone online canada: 200 mg prednisone daily – prednisone 1 mg for sale
how to get amoxicillin over the counter amoxicillin 500mg capsules uk price of amoxicillin without insurance
furosemide 100 mg furosemide 40mg or lasix side effects
https://maps.google.ad/url?q=https://furosemide.guru generic lasix
buy furosemide online lasix 100 mg tablet and furosemide lasix online
https://lisinopril.top/# cost of lisinopril 40 mg
https://stromectol.fun/# buy ivermectin stromectol
can you purchase amoxicillin online: azithromycin amoxicillin – amoxicillin 500 mg without prescription
http://lisinopril.top/# lisinopril 2mg tablet
amoxicillin 500 coupon amoxil generic order amoxicillin online no prescription
5 mg prednisone daily: prednisone in uk – prednisone 21 pack
http://amoxil.cheap/# buy cheap amoxicillin online
https://amoxil.cheap/# amoxicillin 500 coupon
how can i get prednisone online without a prescription prednisone without prescription.net 50 mg prednisone from canada
how to buy lisinopril price lisinopril 20 mg or zestril medicine
http://herna.net/cgi/redir.cgi?lisinopril.top lisinopril in mexico
zestoretic online zestril medication and 60 lisinopril cost lisinopril 50 mg
prednisone tablets 2.5 mg: order prednisone – can i buy prednisone from canada without a script
http://buyprednisone.store/# prednisone 2.5 mg daily
amoxicillin 500mg capsule buy online amoxicillin 500mg capsule or amoxicillin online no prescription
https://maps.google.td/url?sa=t&url=https://amoxil.cheap amoxicillin 500mg price
amoxicillin no prescription generic amoxil 500 mg and amoxicillin from canada purchase amoxicillin online without prescription
buy ivermectin pills ivermectin 500ml ivermectin lotion price
http://amoxil.cheap/# amoxicillin 500mg without prescription
zoloft depression
prednisone online australia prednisone 5093 or prednisone 4mg
https://www.google.gm/url?q=https://buyprednisone.store otc prednisone cream
prednisone without a prescription 20 mg of prednisone and where can i buy prednisone without prescription india buy prednisone online
prednisone 50 mg tablet cost: prednisone cost canada – prednisone uk price
https://amoxil.cheap/# where can you buy amoxicillin over the counter
https://lisinopril.top/# lisinopril 40 mg price
can i purchase amoxicillin online: amoxicillin script – amoxicillin price without insurance
brand prednisone prednisone 4mg tab over the counter prednisone cream
furosemide hypernatremia
http://furosemide.guru/# lasix tablet
lisinopril 20mg prices: where to buy lisinopril – can you buy lisinopril online
https://amoxil.cheap/# cheap amoxicillin 500mg
http://amoxil.cheap/# amoxicillin 500mg without prescription
buy prednisone from canada prednisone 30 mg daily prednisone capsules
lisinopril 20 mg 12.5 mg lisinopril 40 mg price in india lisinopril uk
ivermectin buy australia: ivermectin 6mg – buy ivermectin uk
http://amoxil.cheap/# can i purchase amoxicillin online
lisinopril 20mg
alternatives to flagyl
http://furosemide.guru/# lasix 100 mg tablet
amoxicillin without a prescription: amoxicillin 500 mg without prescription – amoxicillin 500mg price
https://furosemide.guru/# lasix tablet
ivermectin 3mg pill stromectol liquid ivermectin 6
furosemide 100 mg lasix 20 mg or lasix side effects
http://www.derfischkopf.de/url?q=https://furosemide.guru lasix 40 mg
lasix 40 mg furosemide 40 mg and lasix online lasix generic name
http://buyprednisone.store/# prednisone rx coupon
can i buy generic lisinopril online: cheapest price for lisinopril india – lisinopril 3760
http://amoxil.cheap/# medicine amoxicillin 500mg
how much is 30 lisinopril lisinopril 5 mg over the counter can you buy lisinopril online
http://stromectol.fun/# stromectol coronavirus
amoxicillin 750 mg price amoxicillin 500mg no prescription where to buy amoxicillin 500mg without prescription
lisinopril 100 mg: cost for 40 mg lisinopril – lisinopril 40 mg purchase
https://amoxil.cheap/# amoxicillin no prescipion
https://buyprednisone.store/# prednisone medicine
ivermectin 1 cream generic: ivermectin for humans – generic name for ivermectin
lasix 40mg Buy Furosemide lasix furosemide
https://lisinopril.top/# buy cheap lisinopril 40mg
http://lisinopril.top/# lisinopril 60 mg daily
cost of lisinopril 5 mg lisinopril medicine or lisinopril 20 mg uk
https://www.adminer.org/redirect/?url=http://lisinopril.top buy generic lisinopril
20 mg lisinopril tablets lisinopril 10mg daily and cost for 40 mg lisinopril where can i buy zestril
amoxicillin 500 mg tablet price buy amoxicillin 500mg capsules uk or in**@ap**********.com&from=bovecnet&status=0" rel="nofollow ugc">generic amoxicillin online
https://nhatrangclub.vn/proxy.php?link=https://amoxil.cheap can you buy amoxicillin over the counter in canada
amoxicillin order online no prescription order amoxicillin online uk and how much is amoxicillin prescription how to get amoxicillin over the counter
5mg prednisone prednisone in mexico or buy prednisone online paypal
http://www.swdh123.com/url/go.php?url=http://buyprednisone.store prednisone canada prices
no prescription prednisone canadian pharmacy prednisone 5093 and prednisone for sale in canada prednisone in mexico
prinivil coupon: lisinopril tablets for sale – lisinopril 20 mg daily
glucophage minceur
https://buyprednisone.store/# prednisone 54899
ivermectin canada ivermectin syrup buy ivermectin uk
https://stromectol.fun/# stromectol buy
prednisone 100 mg: prednisone 20mg – can you buy prednisone over the counter in canada
http://lisinopril.top/# lisinopril 2 5 mg tablets
prednisone 20mg for sale online order prednisone prednisone uk price
lasix effect on sodium
http://buyprednisone.store/# prednisone 20 mg without prescription
amoxicillin 500mg buy online uk: buy amoxicillin 250mg – how to get amoxicillin
furosemide Buy Lasix furosemide
https://stromectol.fun/# ivermectin goodrx
http://lisinopril.top/# lisinopril 10 mg brand name in india
http://lisinopril.top/# lisinopril 10 mg best price
lisinopril 20mg tablets: lisinopril 0.5 mg – buy cheap lisinopril
gabapentin for bipolar
zithromax lyme
lasix dosage lasix furosemide or lasix furosemide
http://www.studiomassaro.net/popup.asp?foto=public/sponsor/magda copia.jpg&link=furosemide.guru lasix uses
furosemide 40mg furosemida and lasix lasix uses
http://amoxil.cheap/# amoxicillin 500mg without prescription
amoxicillin 500mg buy online canada buy amoxicillin 500mg online amoxicillin 500 capsule
amoxicillin 875 125 mg tab: antibiotic amoxicillin – can i purchase amoxicillin online
http://furosemide.guru/# furosemide 40mg
can you purchase amoxicillin online cost of amoxicillin amoxicillin 500 mg capsule
http://stromectol.fun/# ivermectin 0.5
Yes! Finally something about mobile legends bilet nedir bilet ne işe yarar.
lisinopril 20 mg canadian: lisinopril 25mg tablets – lisinopril 2018
http://lisinopril.top/# lisinopril 3.125
zestril price uk lisinopril cost https://lisinoprilpharm.com/%5Dlisinopril
pharmaceuticals from canada blog link
canadian cialis online pharmacy Canadian Online Pharmacies
amoxicillin 500 mg
Your words have a way of resonating deeply with your readers. Thank you for sharing your wisdom with us. Asheville loves your blog!
http://indianph.com/# Online medicine order
top online pharmacy india
world pharmacy india world pharmacy india reputable indian pharmacies
https://indianph.xyz/# online shopping pharmacy india
indian pharmacy paypal
Your writing style is both engaging and informative. We’re proud to support your blog from Asheville!
https://indianph.xyz/# indianpharmacy com
gabapentin 300mg side effects
https://indianph.com/# legitimate online pharmacies india
top 10 pharmacies in india
mail order pharmacy india reputable indian pharmacies best online pharmacy india
does cephalexin contain sulfa
Online medicine order indian pharmacies safe or india pharmacy mail order
http://www.meetthegreens.org/cgi-registry/bridgepop.pl?url=indianph.com buy medicines online in india
=buy+generic+viagra]reputable indian pharmacies indian pharmacy paypal and top online pharmacy india top 10 pharmacies in india
http://indianph.com/# indianpharmacy com
Online medicine home delivery
http://indianph.xyz/# best online pharmacy india
Online medicine home delivery п»їlegitimate online pharmacies india indian pharmacy
pharmacy website india online shopping pharmacy india or pharmacy website india
https://www.google.com.ni/url?sa=t&url=https://indianph.xyz top online pharmacy india
best india pharmacy top 10 online pharmacy in india and world pharmacy india buy medicines online in india
п»їlegitimate online pharmacies india indian pharmacy online best india pharmacy
http://indianph.xyz/# top 10 pharmacies in india
top 10 online pharmacy in india
escitalopram oxalate 10mg high
http://indianph.com/# indian pharmacies safe
buy prescription drugs from india
https://indianph.xyz/# best online pharmacy india
http://indianph.com/# buy prescription drugs from india
cheapest online pharmacy india
indian pharmacy buy medicines online in india top 10 online pharmacy in india
https://indianph.com/# india pharmacy
top 10 online pharmacy in india
https://indianph.com/# indian pharmacy online
reputable indian pharmacies mail order pharmacy india mail order pharmacy india
top 10 online pharmacy in india pharmacy website india or indianpharmacy com
http://www.nakayama-dr.jp/feed2js2/feed2js.php?src=http://indianph.com indian pharmacy
indian pharmacies safe buy prescription drugs from india and buy medicines online in india cheapest online pharmacy india
world pharmacy india reputable indian pharmacies or best online pharmacy india
http://www.krovatka.ru/f/rr.cgi?http://indianph.com/ reputable indian online pharmacy
Online medicine home delivery buy medicines online in india and indian pharmacies safe online pharmacy india
does ciprofloxacin treat uti
Де купити надійну спецтехніку
спец машини https://spectehnika-sksteh.co.ua .
wegovy online prescription
Having read this I thought it was very informative. I appreciate you taking the time and effort to put this article together. I once again find myself spending way to much time both reading and commenting. But so what, it was still worth it!
http://cipro.guru/# buy cipro online canada
tamoxifen pill tamoxifen moa how does tamoxifen work
raloxifene vs tamoxifen: tamoxifen blood clots – tamoxifen for gynecomastia reviews
https://cipro.guru/# buy ciprofloxacin over the counter
https://nolvadex.guru/# cost of tamoxifen
ciprofloxacin mail online cipro for sale or cipro
https://image.google.ml/url?q=https://cipro.guru buy ciprofloxacin
buy cipro online buy cipro online canada and cipro online no prescription in the usa cipro online no prescription in the usa
https://diflucan.pro/# diflucan 1 pill
over the counter diflucan 150: diflucan 150mg – over the counter diflucan 150
п»їcytotec pills online Abortion pills online Misoprostol 200 mg buy online
https://cytotec24.com/# Misoprostol 200 mg buy online
wegovy tablets buy
tamoxifen adverse effects: tamoxifen reviews – tamoxifen cost
http://cytotec24.shop/# buy cytotec over the counter
cephalexin 500 mg como tomar
doxycycline 100mg dogs doxy 200 buy doxycycline cheap
diflucan medicine diflucan tablets online or diflucan 50 mg capsule
https://www.okpodiatrists.org/external-link?url=https://diflucan.pro diflucan 150 mg over the counter
online rx diflucan medicine diflucan price and diflucan 110 mg can you buy diflucan over the counter in australia
https://nolvadex.guru/# tamoxifen dosage
cytotec buy online usa: order cytotec online – Abortion pills online
http://diflucan.pro/# diflucan 125mg
buy nolvadex online tamoxifen mechanism of action tamoxifen brand name
https://cytotec24.shop/# buy misoprostol over the counter
http://doxycycline.auction/# doxycycline hyclate
doxycycline hyc doxycycline 200 mg or doxycycline 100mg capsules
https://images.google.ml/url?q=https://doxycycline.auction doxycycline hyc
doxylin buy cheap doxycycline online and order doxycycline doxycycline hyclate 100 mg cap
diflucan 150 mg fluconazole: diflucan tablet india – diflucan generic costs
http://diflucan.pro/# diflucan otc uk
buy cheap doxycycline order doxycycline buy doxycycline online without prescription
http://diflucan.pro/# diflucan tablets australia
http://cytotec24.shop/# order cytotec online
http://cipro.guru/# ciprofloxacin generic price
ciprofloxacin buy generic ciprofloxacin п»їcipro generic
buy cipro cheap п»їcipro generic or purchase cipro
http://buttonspace.com/for/cipro.guru cipro
ciprofloxacin order online ciprofloxacin over the counter and buy cipro cheap cipro ciprofloxacin
https://cipro.guru/# buy cipro cheap
http://doxycycline.auction/# buy generic doxycycline
diflucan prescription cost buy diflucan uk diflucan price in india
http://doxycycline.auction/# odering doxycycline
https://cipro.guru/# cipro for sale
https://cipro.guru/# where can i buy cipro online
order cytotec online buy cytotec pills online cheap buy cytotec over the counter
http://abelladanger.online/# Abella Danger
https://abelladanger.online/# abella danger video
Sweetie Fox: Sweetie Fox video – Sweetie Fox
http://abelladanger.online/# abella danger filmleri
http://abelladanger.online/# abella danger video
Sweetie Fox filmleri: Sweetie Fox video – Sweetie Fox filmleri
lana rhoades izle: lana rhoades video – lana rhoades
http://abelladanger.online/# Abella Danger
http://abelladanger.online/# Abella Danger
https://abelladanger.online/# abella danger izle
https://abelladanger.online/# abella danger izle
What’s up, yeah this piece of writing is in fact pleasant and I have learned lot of things from it about blogging. thanks.
https://evaelfie.pro/# eva elfie video
sweety fox: sweety fox – sweety fox
http://evaelfie.pro/# eva elfie izle
https://angelawhite.pro/# Angela White video
https://sweetiefox.online/# swetie fox
Angela White video: Angela White video – ?????? ????
https://sweetiefox.online/# Sweetie Fox modeli
lana rhoades video: lana rhoades – lana rhoades video
http://evaelfie.pro/# eva elfie izle
http://sweetiefox.online/# Sweetie Fox izle
Angela White video: Angela White – ?????? ????
http://evaelfie.pro/# eva elfie izle
https://evaelfie.pro/# eva elfie
http://angelawhite.pro/# Angela White
how to calculate bactrim dose
eva elfie video: eva elfie filmleri – eva elfie filmleri
http://angelawhite.pro/# Angela White filmleri
https://lanarhoades.fun/# lana rhoades video
amoxicillin for strep throat
how to calculate bactrim dose
http://lanarhoades.fun/# lana rhoades
lana rhoades izle: lana rhoades izle – lana rhodes
https://sweetiefox.online/# Sweetie Fox modeli
Angela White: abella danger filmleri – abella danger izle
https://angelawhite.pro/# Angela White
http://sweetiefox.online/# Sweetie Fox
https://sweetiefox.online/# sweety fox
Angela White izle: ?????? ???? – ?????? ????
Sweetie Fox video Sweetie Fox filmleri or Sweetie Fox video
https://matsuden235.jp/index.php?a=free_page/goto_mobile&referer=https://sweetiefox.online swetie fox
sweeti fox swetie fox and sweeti fox Sweetie Fox
https://lanarhoades.fun/# lana rhoades izle
http://abelladanger.online/# abella danger izle
https://angelawhite.pro/# ?????? ????
lana rhodes: lana rhoades video – lana rhoades izle
Sweetie Fox modeli: sweety fox – Sweetie Fox modeli
http://angelawhite.pro/# Angela White
https://sweetiefox.online/# swetie fox
http://sweetiefox.online/# sweeti fox
lana rhoades izle lana rhoades video or lana rhoades izle
https://maps.google.cat/url?sa=t&url=https://lanarhoades.fun lana rhoades video
lana rhodes lana rhodes and lana rhoades filmleri lana rhoades filmleri
Angela White izle: Angela White filmleri – Angela White filmleri
https://evaelfie.pro/# eva elfie
http://abelladanger.online/# abella danger filmleri
Sweetie Fox Sweetie Fox filmleri or Sweetie Fox filmleri
https://cse.google.com.br/url?sa=t&url=https://sweetiefox.online sweety fox
Sweetie Fox filmleri Sweetie Fox video and Sweetie Fox izle Sweetie Fox filmleri
http://lanarhoades.fun/# lana rhoades modeli
http://evaelfie.pro/# eva elfie video
Angela White filmleri: Abella Danger – abella danger izle
https://evaelfie.pro/# eva elfie filmleri
?????? ????: ?????? ???? – Angela White filmleri
cephalexin for acne
http://lanarhoades.fun/# lana rhoades filmleri
https://lanarhoades.fun/# lana rhodes
Angela White video: abella danger video – Abella Danger
https://angelawhite.pro/# Angela Beyaz modeli
http://angelawhite.pro/# Angela White izle
Angela White filmleri Angela White izle or Angela Beyaz modeli
http://images.google.com.bz/url?q=https://angelawhite.pro Angela Beyaz modeli
?????? ???? ?????? ???? and Angela White izle Angela White video
sweety fox: Sweetie Fox video – swetie fox
http://evaelfie.pro/# eva elfie video
https://evaelfie.pro/# eva elfie
sweeti fox: Sweetie Fox filmleri – Sweetie Fox video
Sweetie Fox izle Sweetie Fox video or sweeti fox
http://7ba.info/out.php?url=https://sweetiefox.online Sweetie Fox video
Sweetie Fox izle sweety fox and swetie fox Sweetie Fox video
eva elfie full video: eva elfie hot – eva elfie hd
Hack] Unique A.I. App Makes Us $635/Day
https://www.youtube.com/watch?v=z0aiLF3Sz7E
sweetie fox full video: sweetie fox – sweetie fox full
http://sweetiefox.pro/# sweetie fox new
mia malkova girl mia malkova only fans mia malkova girl
https://sweetiefox.pro/# sweetie fox full
sweetie fox new: sweetie fox full – fox sweetie
eva elfie full videos: eva elfie new videos – eva elfie
https://lanarhoades.pro/# lana rhoades full video
lana rhoades hot lana rhoades solo lana rhoades hot
https://miamalkova.life/# mia malkova photos
sweetie fox cosplay: sweetie fox full video – sweetie fox full video
adult dating sites: https://lanarhoades.pro/# lana rhoades pics
ph sweetie fox: fox sweetie – sweetie fox full
http://miamalkova.life/# mia malkova latest
mia malkova new video mia malkova latest mia malkova only fans
https://miamalkova.life/# mia malkova new video
mia malkova photos: mia malkova full video – mia malkova
neurontin uses for nerve pain
eva elfie full video: eva elfie videos – eva elfie videos
http://evaelfie.site/# eva elfie full video
eva elfie new video eva elfie videos eva elfie full video
sweetie fox video: sweetie fox – sweetie fox video
sweetie fox cosplay: ph sweetie fox – sweetie fox full video
http://lanarhoades.pro/# lana rhoades hot
who is brent rivera dating: https://lanarhoades.pro/# lana rhoades unleashed
sweetie fox new: sweetie fox video – sweetie fox new
eva elfie new videos: eva elfie new videos – eva elfie new videos
https://lanarhoades.pro/# lana rhoades unleashed
lana rhoades unleashed lana rhoades full video lana rhoades full video
side effects of escitalopram and alcohol
http://lanarhoades.pro/# lana rhoades pics
mia malkova girl: mia malkova girl – mia malkova new video
eva elfie hot: eva elfie – eva elfie new videos
lana rhoades videos lana rhoades full video or lana rhoades hot
https://cse.google.dj/url?sa=t&url=https://lanarhoades.pro lana rhoades
lana rhoades videos lana rhoades boyfriend and lana rhoades lana rhoades
eva elfie hd: eva elfie hot – eva elfie new videos
http://miamalkova.life/# mia malkova movie
lana rhoades pics lana rhoades full video lana rhoades boyfriend
best dating site: https://miamalkova.life/# mia malkova movie
http://lanarhoades.pro/# lana rhoades full video
eva elfie hd: eva elfie photo – eva elfie hot
sweetie fox sweetie fox cosplay or ph sweetie fox
http://www.glasscontrol.co.uk/gallery/main.php?g2_view=core.UserAdmin&g2_subView=core.UserRecoverPassword&g2_return=https://sweetiefox.pro sweetie fox video
sweetie fox fox sweetie and sweetie fox full sweetie fox video
mia malkova new video mia malkova videos or mia malkova movie
https://images.google.cz/url?sa=t&url=http://miamalkova.life mia malkova latest
mia malkova new video mia malkova new video and mia malkova photos mia malkova latest
sweetie fox full: sweetie fox new – sweetie fox video
https://lanarhoades.pro/# lana rhoades solo
lana rhoades hot lana rhoades videos lana rhoades solo
https://miamalkova.life/# mia malkova videos
sweetie fox cosplay: sweetie fox – sweetie fox
mia malkova only fans: mia malkova videos – mia malkova new video
free online dating and personals: https://evaelfie.site/# eva elfie videos
mia malkova girl: mia malkova new video – mia malkova photos
https://sweetiefox.pro/# sweetie fox new
eva elfie photo eva elfie hd eva elfie hd
lana rhoades full video: lana rhoades hot – lana rhoades solo
http://sweetiefox.pro/# sweetie fox
eva elfie full videos eva elfie videos or eva elfie
https://images.google.com.ph/url?q=https://evaelfie.site eva elfie full videos
eva elfie videos eva elfie new videos and eva elfie eva elfie photo
sweetie fox cosplay: sweetie fox full – sweetie fox
https://evaelfie.site/# eva elfie hot
sweetie fox [url=https://sweetiefox.pro/#]fox sweetie[/url] sweetie fox new
mia malkova full video: mia malkova girl – mia malkova videos
http://sweetiefox.pro/# sweetie fox
chinese dating show: https://lanarhoades.pro/# lana rhoades solo
mia malkova photos: mia malkova photos – mia malkova movie
mia malkova hd: mia malkova new video – mia malkova new video
https://lanarhoades.pro/# lana rhoades full video
mia malkova hd mia malkova girl mia malkova movie
sweetie fox new: sweetie fox video – sweetie fox
http://sweetiefox.pro/# sweetie fox cosplay
lana rhoades unleashed lana rhoades videos or lana rhoades unleashed
https://cse.google.com.ua/url?q=https://lanarhoades.pro lana rhoades
lana rhoades hot lana rhoades hot and lana rhoades hot lana rhoades hot
eva elfie full videos: eva elfie photo – eva elfie new videos
https://miamalkova.life/# mia malkova photos
mia malkova mia malkova movie mia malkova
https://miamalkova.life/# mia malkova girl
dating services online: http://sweetiefox.pro/# sweetie fox full
mia malkova only fans mia malkova videos or mia malkova
http://leefirstbaptistchurch.org/System/Login.asp?id=48747&Referer=http://miamalkova.life mia malkova only fans
mia malkova hd mia malkova new video and mia malkova full video mia malkova movie
mia malkova latest: mia malkova latest – mia malkova only fans
mia malkova hd: mia malkova latest – mia malkova full video
mia malkova: mia malkova movie – mia malkova latest
https://lanarhoades.pro/# lana rhoades pics
sweetie fox full video fox sweetie sweetie fox full
http://miamalkova.life/# mia malkova hd
mia malkova full video: mia malkova videos – mia malkova only fans
aviator bet: aviator betting game – aviator game
https://pinupcassino.pro/# cassino pin up
pin-up casino login pin up pin-up cassino
aviator: aviator – play aviator
https://aviatoroyunu.pro/# pin up aviator
citalopram for depression
https://aviatormalawi.online/# aviator game
what is cozaar 25 mg used for
cassino pin up: cassino pin up – pin up cassino online
como jogar aviator: aviator online – aviator online
jogar aviator online: aviator pin up – pin up aviator
https://aviatormalawi.online/# aviator game
https://jogodeaposta.fun/# ganhar dinheiro jogando
aviator aviator sinyal hilesi aviator sinyal hilesi
https://pinupcassino.pro/# pin-up casino entrar
aviator oyna: aviator oyunu – aviator oyunu
stability of ddavp for iv
aviator: pin up aviator – aviator bahis
https://aviatoroyunu.pro/# aviator
aviator betting game: aviator malawi – play aviator
http://aviatormocambique.site/# aviator online
site de apostas: aplicativo de aposta – ganhar dinheiro jogando
depakote dosing for bipolar
aviator moçambique: aviator moçambique – aviator online
aviator jogo jogar aviator online or estrela bet aviator
https://images.google.kg/url?q=https://aviatorjogar.online aviator game
jogar aviator Brasil aviator jogo and estrela bet aviator aviator game
ganhar dinheiro jogando: jogo de aposta online – ganhar dinheiro jogando
https://aviatorjogar.online/# jogar aviator Brasil
http://jogodeaposta.fun/# site de apostas
cassino pin up cassino pin up pin up casino
https://aviatormocambique.site/# como jogar aviator em mocambique
aviator game: aviator bet malawi – aviator malawi
aplicativo de aposta melhor jogo de aposta or melhor jogo de aposta para ganhar dinheiro
http://n-organic.jp/shop/display_cart?return_url=http://jogodeaposta.fun ganhar dinheiro jogando
deposito minimo 1 real melhor jogo de aposta and jogo de aposta aviator jogo de aposta
https://aviatorghana.pro/# aviator sportybet ghana
pin up aviator: aviator – aviator oyna
aviator game online: aviator betting game – aviator ghana
http://aviatorjogar.online/# aviator jogar
aviator bet aviator game bet aviator ghana
aviator oyna: aviator hilesi – aviator oyna
aviator: aviator bet – aviator bet
como jogar aviator em mocambique: como jogar aviator em mocambique – como jogar aviator em mocambique
depósito mínimo 1 real: site de apostas – melhor jogo de aposta
aviator bet: aviator bet – jogar aviator online
pin up aviator: pin up aviator – aviator bahis
aviator oyna: aviator – aviator oyna
cassino pin up cassino pin up or pin up bet
http://emaame.com/redir.cgi?url=https://pinupcassino.pro aviator oficial pin up
pin up aviator pin-up casino and pin-up casino entrar aviator oficial pin up
http://aviatormalawi.online/# aviator game online
aviator jogo estrela bet aviator aviator betano
zithromax cost uk: how much does zithromax cost cheap zithromax pills
jogar aviator online: aviator betano – jogar aviator Brasil
jogar aviator online: aviator pin up – aviator jogar
https://aviatorghana.pro/# aviator game online
aviator game online: aviator – aviator betting game
purchase zithromax online – https://azithromycin.pro/zithromax-pill-id.html zithromax 500mg over the counter
pin up aviator: estrela bet aviator – jogar aviator Brasil
https://aviatorjogar.online/# aviator pin up
online pharmacy pain medicine
estrela bet aviator: aviator jogo – aviator betano
zithromax 500 mg lowest price pharmacy online: zithromax and birth control pill zithromax 500mg
ganhar dinheiro jogando jogo de aposta online or aplicativo de aposta
https://images.google.com.mm/url?q=https://jogodeaposta.fun site de apostas
site de apostas aviator jogo de aposta and melhor jogo de aposta melhor jogo de aposta
aviator betano jogar aviator Brasil or aviator jogo
http://envirodesic.com/healthyschools/commpost/hstransition.asp?urlrefer=aviatorjogar.online aviator jogar
aviator betano pin up aviator and aviator game aviator bet
aviator betting game: aviator betting game – aviator bet malawi login
reputable indian pharmacies online pharmacy usa online pharmacy india indianpharm.store
best online pharmacy india: online pharmacy usa – world pharmacy india indianpharm.store
blood pressure medicine cozaar
indian trail pharmacy
reputable mexican pharmacies online: mexican pharmacy – mexican border pharmacies shipping to usa mexicanpharm.shop
buy drugs from canada best rated canadian pharmacy best canadian online pharmacy reviews canadianpharm.store
paxil vs citalopram
indianpharmacy com: Online medicine home delivery – indianpharmacy com indianpharm.store
https://indianpharm24.shop/# best online pharmacy india indianpharm.store
http://mexicanpharm24.shop/# medication from mexico pharmacy mexicanpharm.shop
https://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
canadian pharmacy mall: Pharmacies in Canada that ship to the US – canada pharmacy canadianpharm.store
canadian pharmacy phone number Canada pharmacy online legitimate canadian mail order pharmacy canadianpharm.store
depakote davis pdf
Online medicine home delivery: indian pharmacy – world pharmacy india indianpharm.store
the canadian pharmacy canadian drugs or escrow pharmacy canada
https://images.google.gy/url?sa=t&url=https://canadianpharmlk.shop best rated canadian pharmacy
canadian pharmacy meds review canadianpharmacy com and safe reliable canadian pharmacy my canadian pharmacy review
http://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
https://indianpharm24.com/# indian pharmacy paypal indianpharm.store
ddavp coagulation
https://mexicanpharm24.com/# best mexican online pharmacies mexicanpharm.shop
https://mexicanpharm24.shop/# reputable mexican pharmacies online mexicanpharm.shop
online shopping pharmacy india: buy prescription drugs from india – top 10 online pharmacy in india indianpharm.store
best online pharmacies in mexico mexican pharmaceuticals online or buying prescription drugs in mexico online
http://velikanrostov.ru/bitrix/redirect.php?event1=&event2=&event3=&goto=https://mexicanpharm24.com mexican mail order pharmacies
buying prescription drugs in mexico online mexican border pharmacies shipping to usa and reputable mexican pharmacies online best online pharmacies in mexico
https://indianpharm24.com/# online pharmacy india indianpharm.store
http://canadianpharmlk.com/# canada pharmacy 24h canadianpharm.store
https://mexicanpharm24.com/# mexico pharmacies prescription drugs mexicanpharm.shop
the canadian pharmacy: CIPA approved pharmacies – canadian pharmacy online ship to usa canadianpharm.store
best online canadian pharmacy International Pharmacy delivery recommended canadian pharmacies canadianpharm.store
mexico pharmacy: order online from a Mexican pharmacy – mexico drug stores pharmacies mexicanpharm.shop
http://indianpharm24.shop/# indian pharmacy indianpharm.store
mexico drug stores pharmacies mexico pharmacies prescription drugs or mexican pharmaceuticals online
http://lonevelde.lovasok.hu/out_link.php?url=https://mexicanpharm24.com purple pharmacy mexico price list
mexican online pharmacies prescription drugs mexican pharmaceuticals online and mexico drug stores pharmacies mexico drug stores pharmacies
https://mexicanpharm24.shop/# mexico pharmacy mexicanpharm.shop
canadian pharmacy online store my canadian pharmacy reviews or canadian drugs
http://www.google.com.cu/url?q=https://canadianpharmlk.shop/ legit canadian pharmacy online
safe canadian pharmacy canadian pharmacy and best canadian online pharmacy northwest canadian pharmacy
http://canadianpharmlk.shop/# is canadian pharmacy legit canadianpharm.store
canadian pharmacy: My Canadian pharmacy – canada cloud pharmacy canadianpharm.store
https://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
http://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
canada rx pharmacy world: canadian pharmacy – canada pharmacy world canadianpharm.store
http://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
mexico pharmacies prescription drugs: Mexico pharmacy price list – buying prescription drugs in mexico online mexicanpharm.shop
pharmacy website india online pharmacy usa pharmacy website india indianpharm.store
Мы эксперты SEO-экспертов, занимающихся увеличением посещаемости и рейтинга вашего сайта в поисковых системах.
Мы постигли успехи в своей области и расширим ваш кругозор нашим опытом и знаниями.
Какие преимущества вы получите:
• услуги продвижения сайта в поисковых системах
• Тщательный анализ вашего сайта и разработка персональной стратегии продвижения.
• Оптимизация контента и технических аспектов вашего сайта для максимальной эффективности.
• Систематический мониторинг и анализ результатов с целью улучшения вашего онлайн-присутствия.
Подробнее https://seo-prodvizhenie-ulyanovsk1.ru/
Уже много клиентов оценили результаты: рост посещаемости, улучшение позиций в поисковых системах и, конечно, рост бизнеса. У нас есть возможность предоставить вам бесплатную консультацию, для обсуждения ваших требований и разработки стратегии продвижения, соответствующей вашим целям и бюджету.
Не упустите возможность улучшить свой бизнес в онлайн-мире. Свяжитесь с нами немедленно.
https://indianpharm24.com/# india pharmacy mail order indianpharm.store
http://canadianpharmlk.com/# legitimate canadian pharmacy online canadianpharm.store
medication from mexico pharmacy mexico drug stores pharmacies or medication from mexico pharmacy
https://images.google.com.ng/url?sa=t&url=https://mexicanpharm24.shop mexico drug stores pharmacies
mexican border pharmacies shipping to usa mexico pharmacy and mexican online pharmacies prescription drugs medicine in mexico pharmacies
where to buy cheap clomid without rx: online doctor to prescribe clomid – where can i buy clomid without prescription
order clomid price: clomid 50mg price – where buy cheap clomid without rx
I think what you published made a bunch of sense. But, consider this, suppose you were to write a killer headline? I am not saying your information isn’t solid., but suppose you added something that makes people want more? I mean Drug & Alcohol Addiction Treatment Resources is a little vanilla. You might look at Yahoo’s home page and note how they create news titles to grab viewers to click. You might add a related video or a related pic or two to get people interested about everything’ve written. Just my opinion, it might bring your posts a little livelier.
https://amoxilst.pro/# purchase amoxicillin 500 mg
prednisone without prescription 10mg: alcohol and prednisone – where can i buy prednisone without a prescription
can i order cheap clomid pill: clomid and progesterone – buy clomid
order prednisone 100g online without prescription can i buy prednisone online in uk prednisone over the counter cost
augmentin 875 price
https://prednisonest.pro/# prednisone cost canada
can you buy prednisone over the counter in usa: what is the lowest dose of prednisone you can take – apo prednisone
prednisone 40 mg: can you buy prednisone over the counter in canada – prednisone 60 mg price
https://clomidst.pro/# clomid without rx
prednisone 5093: prednisolone vs prednisone – prednisone pill prices
amoxicillin 500mg for sale uk: amoxicillin 500mg how to take – how to get amoxicillin over the counter
nice guidelines ezetimibe
buy amoxicillin 250mg: amoxicillin 500 tablet – where can you buy amoxicillin over the counter
http://prednisonest.pro/# can i buy prednisone online without prescription
how to buy cheap clomid now can you get generic clomid without rx or where can i buy cheap clomid without prescription
https://www.google.dk/url?q=https://clomidst.pro buy clomid without rx
generic clomid without prescription can i purchase clomid without insurance and how to buy clomid online can you get generic clomid without rx
prednisone over the counter australia prednisone price canada prednisone pill 10 mg
prednisone 10 tablet: prednisone dose pack – prednisone 10mg for sale
diclofenac sodium topical gel 1 reviews
can i buy generic clomid: can i order clomid pills – can you get clomid without prescription
https://amoxilst.pro/# 875 mg amoxicillin cost
how to buy cheap clomid price: pct clomid – buying clomid without prescription
prednisone pak: prednisone high – prednisone pharmacy prices
cartia xt vs diltiazem er
prednisone 80 mg daily prednisone 2.5 mg price or prednisone brand name india
http://www.allspare.ru/redirect.php?id=1&url=prednisonest.pro prednisone 5 mg cheapest
prednisone prescription for sale prednisone without prescription and purchase prednisone 10mg prednisone 50 mg price
rexall pharmacy amoxicillin 500mg: amoxicillin generic – where can i get amoxicillin
https://amoxilst.pro/# amoxicillin 500 mg
amoxicillin 250 mg: can you buy amoxicillin over the counter in canada – amoxicillin medicine
http://www.one-xbet-france.com
Plateforme en ligne 1xBet: outils discharge gagner de l’argent. En general, 1xBet France est un bookmaker classique talk up comme risk365 bookmaker et beaucoup d’autres.
http://www.one-xbet-france.com
order cheap clomid without dr prescription: clomid ovulation calculator – cost of generic clomid pills
buy prednisone 10mg prednisone brand name us prednisone 300mg
cost clomid pills: clomid cheap – where to buy clomid
top rated ed pills: low cost ed medication – boner pills online
This story is from November 26, 2020 Filed Under: Gameschooling Tagged With: 2-player games, games for couples, Gameschooling, two-player games Enjoy our collection of betting games, they are the life of any social gathering, player with the best cards wins, proud to support large gatherings as all of our other games! Copyright ©2002-2023 Armand Niculescu Media Division srl. All rights reserved.Sparkchess is Registered Trademark of Armand Niculescu *Best RUN Game to play *Unlock The Magical Pony Unicorn Characters *Play as 10 Different Unicorns in Cool & Cute Colors *Collect Coins & Get Hearts to Upgrade *Open Surprises & Exclusive Rewards in this running game *Enjoyable KIDS run game adventure *Escape from Obstacles with Hover board, Wings etc *10 magical Howe boards *Avail super cool offers for purchases *Collect & Upgrade Loads of Awesome Powerups *FREE Updates, New Characters Added Regularly *Amazing HD Graphics
https://arthurzlvl266988.onzeblog.com/23978504/people-playing-dominoes
Local co-op is at its best in Cuphead: The Delicious Last Course, the meaty expansion to the original Cuphead game. With Ms. Chalice thrown into the mix, new skills to master, and some of the best boss fights to ever grace a TV screen, The Delicious Last Course doesn’t hold anything back when it starts serving a white-knuckle ride of fun. Having a partner to split the stress makes for an even more exciting experience, and the rest of this DLC is a superb showcase of polished action and amazing art direction. Lethal Company well and truly took Steam by storm during late 2023, surpassing some of the years biggest and best games, and for good reason. This game might look old and haggered, but that’s all part of its stylistic charm and one of many reasons why this survival horror co-op game is relatively refreshing.
prescription drugs online: online pharmacy india – cheapest pharmacy to fill prescriptions without insurance
pharmacy no prescription required order medication without prescription online meds without prescription
flomax generic effectiveness
cheap ed pills online: cheapest online ed treatment – ed pills
edmeds: edmeds – cheapest ed online
cheapest ed online: buy erectile dysfunction treatment – how to get ed meds online
https://onlinepharmacy.cheap/# pharmacy without prescription
order medication without prescription: buying prescription drugs online from canada – buy medication online with prescription
effexor vs lexapro
ed online meds: buy ed pills online – buy ed medication online
online pharmacy without prescription: best online pharmacy – canadian pharmacy coupon code
http://onlinepharmacy.cheap/# cheap pharmacy no prescription
cheapest ed pills online ed medicine or discount ed meds
https://usachannel.info/amankowww/url.php?url=https://edpills.guru best online ed pills
erectile dysfunction pills online discount ed pills and erectile dysfunction medication online cheapest erectile dysfunction pills
buy prescription drugs online without doctor no prescription medicine buying prescription drugs online canada
I am impressed with this internet site, real I am a fan.
canada online pharmacy no prescription: canada online pharmacy – canadian pharmacies not requiring prescription
what is flexeril
canada prescriptions by mail: canadian pharmacy no prescription needed – buying prescription drugs online without a prescription
erection pills online: cheap ed drugs – ed meds by mail
how to get a prescription in canada: online meds without prescription – prescription drugs online canada
online erectile dysfunction medication: buy ed medication online – best ed pills online
art 7 lei de contravencoes penais
non prescription pharmacy pills no prescription or order prescription from canada
https://images.google.sc/url?q=https://pharmnoprescription.pro buying prescription drugs online without a prescription
prescription from canada canadian prescriptions in usa and buy drugs online no prescription canada prescription online
http://edpills.guru/# cheap ed meds
drugstore com online pharmacy prescription drugs: canada pharmacy online – mail order prescription drugs from canada
ed drugs online: cheap ed medicine – boner pills online
discount prescription drugs canada: online pharmacies no prescription – canada pharmacy without prescription
http://mexicanpharm.online/# mexican border pharmacies shipping to usa
http://pharmacynoprescription.pro/# buy medications without a prescription
amitriptyline 150 mg
indianpharmacy com: Online medicine home delivery – Online medicine order
buy prescription drugs on line canadian prescription canadian pharmacy no prescription needed
https://mexicanpharm.online/# mexico pharmacy
medication from mexico pharmacy: mexico drug stores pharmacies – mexico pharmacy
turmeric and allopurinol
https://mexicanpharm.online/# mexican pharmaceuticals online
buying drugs from canada: canadian drug pharmacy – vipps canadian pharmacy
http://indianpharm.shop/# world pharmacy india
I found your blog website on google and examine a couple of of your early posts. Proceed to maintain up the excellent operate. I simply additional up your RSS feed to my MSN Information Reader. Searching for ahead to reading extra from you in a while!…
escrow pharmacy canada: vipps approved canadian online pharmacy – canadian pharmacy online ship to usa
indian pharmacy paypal: reputable indian pharmacies – indianpharmacy com
mexican pharmaceuticals online mexico drug stores pharmacies or buying prescription drugs in mexico
http://www.collegeboyspank.com/Home.aspx?returnurl=http://mexicanpharm.online/ buying prescription drugs in mexico
mexican border pharmacies shipping to usa buying prescription drugs in mexico and best online pharmacies in mexico mexican rx online
canadianpharmacymeds canadian pharmacy king pharmacy canadian superstore
www canadianonlinepharmacy: canadian pharmacy meds – best online canadian pharmacy
https://canadianpharm.guru/# canada pharmacy online
what is the brand name for aripiprazole
no prescription pharmacy online: buy pills without prescription – online pharmacy without prescription
pharmacies in mexico that ship to usa: mexican mail order pharmacies – mexican mail order pharmacies
aspirin tablets
http://indianpharm.shop/# Online medicine home delivery
pharmacy in canada: legal to buy prescription drugs from canada – canadapharmacyonline
http://mexicanpharm.online/# mexico drug stores pharmacies
buying prescription drugs online canada online pharmacy that does not require a prescription or order prescription drugs online without doctor
https://www.google.com.cy/url?sa=t&url=https://pharmacynoprescription.pro no prescription needed
canada prescription canada pharmacy without prescription and no prescription order medication without prescription
mexican pharmacy: medication from mexico pharmacy – buying prescription drugs in mexico online
onlinepharmaciescanada com: canadian pharmacy tampa – canadian neighbor pharmacy
http://mexicanpharm.online/# mexican rx online
canadian king pharmacy: cheapest pharmacy canada – canadapharmacyonline
best online pharmacy no prescription canadian pharmacy no prescription required canadian pharmacy online no prescription needed
mexico drug stores pharmacies mexico pharmacies prescription drugs or mexico pharmacy
https://www.google.com.sl/url?sa=t&url=https://mexicanpharm.online buying prescription drugs in mexico online
mexican pharmaceuticals online п»їbest mexican online pharmacies and mexico drug stores pharmacies reputable mexican pharmacies online
best india pharmacy india pharmacy or best india pharmacy
http://sotofone.ru/bitrix/rk.php?goto=http://indianpharm.shop/ indian pharmacy paypal
best online pharmacy india reputable indian online pharmacy and online shopping pharmacy india indian pharmacies safe
indian pharmacy online: best india pharmacy – reputable indian pharmacies
canadian online drugs: canadian pharmacy price checker – canada drugs reviews
http://mexicanpharm.online/# purple pharmacy mexico price list
no prescription medicine: buy meds online no prescription – best online pharmacy that does not require a prescription in india
http://indianpharm.shop/# indian pharmacy
http://pharmacynoprescription.pro/# no prescription needed
canada prescription: canada prescription drugs online – online pharmacies no prescription
buy medications without prescriptions: best website to buy prescription drugs – online pharmacy without prescription
vipps canadian pharmacy canadian pharmacy no rx needed or global pharmacy canada
https://maps.google.com.hk/url?sa=t&url=https://canadianpharm.guru ordering drugs from canada
canadian pharmacy 24h com my canadian pharmacy rx and canadian pharmacy oxycodone certified canadian international pharmacy
online pharmacy india: cheapest online pharmacy india – indian pharmacy
pharmacy website india world pharmacy india buy prescription drugs from india
http://mexicanpharm.online/# mexico drug stores pharmacies
online pharmacy india: indian pharmacy paypal – online pharmacy india
pharmacies in mexico that ship to usa: buying prescription drugs in mexico – buying from online mexican pharmacy
mexican mail order pharmacies mexican pharmaceuticals online or best online pharmacies in mexico
http://maps.google.com.na/url?q=https://mexicanpharm.online buying prescription drugs in mexico online
purple pharmacy mexico price list buying from online mexican pharmacy and mexican mail order pharmacies pharmacies in mexico that ship to usa
http://indianpharm.shop/# online pharmacy india
buy prescription drugs from india: Online medicine home delivery – reputable indian online pharmacy
https://pharmacynoprescription.pro/# canadian prescriptions in usa
online canadian pharmacy no prescription: online drugstore no prescription – online prescription canada
indian pharmacy online: indian pharmacy – reputable indian pharmacies
https://mexicanpharm.online/# buying prescription drugs in mexico online
maple leaf pharmacy in canada: vipps canadian pharmacy – canada pharmacy online legit
Spot on with this write-up, I really assume this website wants rather more consideration. I’ll most likely be once more to learn way more, thanks for that info.
canada drugs without prescription best online prescription canada online prescription
canadian prescriptions in usa: online meds without prescription – canadian prescription
bupropion xl 150 mg side effects
canada mail order prescription: online pharmacy with prescription – prescription canada
online pharmacies without prescriptions no prescription medicine or canada pharmacies online prescriptions
http://bridge1.ampnetwork.net/?key=1006540158.1006540255&url=https://pharmacynoprescription.pro online drugstore no prescription
mexico online pharmacy prescription drugs medications online without prescriptions and online pharmacy without prescription best online pharmacy that does not require a prescription in india
reputable indian online pharmacy: top 10 pharmacies in india – online pharmacy india
buying prescription drugs in mexico online medication from mexico pharmacy or <a href=" http://werbung-on-demand.net/phpinfo.php?a=cialis+tadalafil “>pharmacies in mexico that ship to usa
https://maps.google.com.kw/url?q=https://mexicanpharm.online buying prescription drugs in mexico
mexico pharmacy mexican drugstore online and mexico drug stores pharmacies buying prescription drugs in mexico
non prescription online pharmacy: buying prescription drugs in india – no prescription drugs online
https://canadianpharm.guru/# canadian pharmacy near me
does celebrex have sulfa in it
http://mexicanpharm.online/# buying prescription drugs in mexico
world pharmacy india reputable indian online pharmacy or pharmacy website india
http://easyhyperlinks.com/index.asp?target=http://indianpharm.shop&displaytext=merchants&submitted=True&submit=Construct+Link indian pharmacies safe
reputable indian online pharmacy top online pharmacy india and world pharmacy india best india pharmacy
indianpharmacy com: india pharmacy mail order – india online pharmacy
canada pharmacy: trustworthy canadian pharmacy – pharmacy in canada
http://indianpharm.shop/# pharmacy website india
canadapharmacyonline: canadianpharmacyworld com – vipps canadian pharmacy
medications online without prescription online pharmacy that does not require a prescription online meds without prescription
medicine in mexico pharmacies: buying prescription drugs in mexico online – buying prescription drugs in mexico
http://pharmacynoprescription.pro/# meds online without prescription
best rated canadian pharmacy: canadian pharmacy india – canadian pharmacy meds
baclofen abuse
pharmacy rx world canada best online canadian pharmacy or canadian pharmacy in canada
http://anonim.co.ro/?canadianpharm.guru canadian drugs pharmacy
ordering drugs from canada canadian pharmacies compare and legitimate canadian pharmacy online best rated canadian pharmacy
augmentin treats
http://pinupgiris.fun/# pin-up bonanza
oyun siteleri slot slot siteleri 2024 en guvenilir slot siteleri
https://aviatoroyna.bid/# aviator sinyal hilesi ucretsiz
http://slotsiteleri.guru/# en iyi slot siteleri
aviator oyunu 50 tl: aviator oyna 100 tl – aviator nas?l oynan?r
http://pinupgiris.fun/# pin-up casino
http://aviatoroyna.bid/# aviator nas?l oynan?r
sweet bonanza yasal site sweet bonanza 100 tl guncel sweet bonanza
deneme bonusu veren siteler: yasal slot siteleri – deneme bonusu veren siteler
aviator oyna 20 tl: aviator oyna 100 tl – aviator oyunu giris
http://aviatoroyna.bid/# aviator hile
http://gatesofolympus.auction/# gates of olympus guncel
aviator oyunu 50 tl aviator oyna 20 tl aviator oyunu 10 tl
http://gatesofolympus.auction/# gates of olympus demo oyna
sweet bonanza bahis: sweet bonanza 100 tl – sweet bonanza demo turkce
http://slotsiteleri.guru/# slot casino siteleri
http://pinupgiris.fun/# pin up indir
aviator hilesi aviator sinyal hilesi aviator sinyal hilesi apk
https://pinupgiris.fun/# pin up indir
bonus veren casino slot siteleri: guvenilir slot siteleri – casino slot siteleri
en iyi slot siteleri 2024: slot siteleri guvenilir – deneme bonusu veren siteler
https://pinupgiris.fun/# pin up giris
sweet bonanza slot demo sweet bonanza yasal site or sweet bonanza demo oyna
http://www.google.ga/url?q=https://sweetbonanza.bid sweet bonanza demo turkce
sweet bonanza giris sweet bonanza yorumlar and sweet bonanza 90 tl sweet bonanza kazanma saatleri
https://slotsiteleri.guru/# bonus veren casino slot siteleri
aviator casino oyunu aviator hilesi ucak oyunu bahis aviator
http://pinupgiris.fun/# pin up casino indir
get high on buspirone
aviator sinyal hilesi apk: aviator sinyal hilesi ucretsiz – aviator oyna 20 tl
drug test products https://forums.dieviete.lv/profils/127605/forum/ baby cough remedies
https://pinupgiris.fun/# pin up
http://sweetbonanza.bid/# sweet bonanza yorumlar
aviator oyunu aviator oyunu aviator oyna 20 tl
celecoxib selective cox 2 inhibitor
http://slotsiteleri.guru/# slot oyun siteleri
aviator sinyal hilesi ucretsiz: aviator oyna slot – aviator oyunu
gates of olympus 1000 demo gates of olympus taktik or gates of olympus nas?l para kazanilir
https://maps.google.com.tw/url?q=https://gatesofolympus.auction gates of olympus demo
gates of olympus demo turkce oyna gates of olympus oyna demo and gates of olympus demo turkce gates of olympus oyna demo
http://slotsiteleri.guru/# 2024 en iyi slot siteleri
pragmatic play gates of olympus gates of olympus slot gates of olympus taktik
http://gatesofolympus.auction/# gates of olympus hilesi
https://sweetbonanza.bid/# sweet bonanza siteleri
aviator oyna 20 tl: aviator oyunu – aviator oyna 20 tl
gates of olympus max win: gates of olympus oyna demo – gates of olympus oyna demo
sweet bonanza guncel sweet bonanza giris or sweet bonanza
http://2ch.io/sweetbonanza.bid sweet bonanza slot demo
sweet bonanza oyna sweet bonanza hilesi and pragmatic play sweet bonanza sweet bonanza yasal site
http://pinupgiris.fun/# pin-up casino indir
http://slotsiteleri.guru/# en iyi slot siteleri
yeni slot siteleri en cok kazandiran slot siteleri deneme bonusu veren slot siteleri
http://sweetbonanza.bid/# sweet bonanza taktik
sweet bonanza free spin demo: sweet bonanza – sweet bonanza kazanc
ashwagandha mayo clinic
http://gatesofolympus.auction/# gates of olympus max win
anxiety medication celexa
buying from canadian pharmacies
https://slotsiteleri.guru/# slot casino siteleri
gates of olympus demo free spin gates of olympus oyna demo gates of olympus max win
pin up aviator: pin up giris – pin up casino
pin up indir: pin up casino giris – pin up
http://pinupgiris.fun/# aviator pin up
pin up aviator pin up casino indir or pin-up online
https://www.google.cg/url?q=https://pinupgiris.fun pin-up casino
pin up aviator pin up giris and pin-up casino giris pin-up giris
https://gatesofolympus.auction/# gates of olympus oyna demo
https://pinupgiris.fun/# pin-up casino
aviator sinyal hilesi ucretsiz aviator hile ucak oyunu bahis aviator
aviator: aviator ucak oyunu – aviator giris
http://gatesofolympus.auction/# gates of olympus oyna
sweet bonanza indir guncel sweet bonanza or sweet bonanza siteleri
https://www.textise.net/showText.aspx?strURL=http://sweetbonanza.bid sweet bonanza free spin demo
sweet bonanza hilesi sweet bonanza kazanma saatleri and guncel sweet bonanza pragmatic play sweet bonanza
deneme veren slot siteleri en yeni slot siteleri or slot siteleri 2024
https://cse.google.com.do/url?q=http://slotsiteleri.guru bonus veren slot siteleri
guvenilir slot siteleri 2024 slot kumar siteleri and slot siteleri 2024 yasal slot siteleri
https://slotsiteleri.guru/# en çok kazandiran slot siteleri
Hey! I know this is kinda off topic but I was wondering if you knew where I could locate a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
Hiya, I am really glad I’ve found this info. Nowadays bloggers publish just about gossips and net and this is really frustrating. A good website with exciting content, that’s what I need. Thank you for keeping this website, I will be visiting it. Do you do newsletters? Cant find it.
great issues altogether, you simply received a new reader. What would you suggest in regards to your submit that you simply made a few days ago? Any certain?
gates of olympus nas?l para kazanilir: gates of olympus nas?l para kazanilir – gates of olympus demo turkce oyna
buy prescription drugs from canada cheap canadian mail order pharmacy canadian pharmacy reviews
online pharmacy non prescription drugs
indian pharmacy online: Generic Medicine India to USA – top 10 pharmacies in india
mexican mail order pharmacies mexican pharmacy mexican online pharmacies prescription drugs
http://indianpharmacy.icu/# top 10 online pharmacy in india
reputable indian pharmacies indian pharmacy world pharmacy india
canadapharmacyonline legit: canadian pharmacy tampa – canadian pharmacy online
mexican pharmaceuticals online: mexico pharmacy – mexico drug stores pharmacies
canadian pharmacy com canadian pharmacy 24 canadianpharmacyworld com
medicine in mexico pharmacies: Mexican Pharmacy Online – medication from mexico pharmacy
http://indianpharmacy.icu/# indian pharmacy online
drugs from canada canadian pharmacy prices or canadian pharmacies comparison
https://www.google.mn/url?sa=t&url=https://canadianpharmacy24.store canadian pharmacies online
canadian pharmacy no rx needed canadian pharmacy ltd and canadian drug pharmacy safe online pharmacies in canada
best online pharmacies in mexico: Online Pharmacies in Mexico – buying prescription drugs in mexico online
canada drug pharmacy: Large Selection of Medications – canadian pharmacy online store
buy medicines online in india Healthcare and medicines from India buy medicines online in india
canadian pharmacy in canada: canadian pharmacy 24 – pharmacy com canada
best india pharmacy: Cheapest online pharmacy – indian pharmacy
pharmacy website india indian pharmacy top 10 online pharmacy in india
mexican online pharmacies prescription drugs mexico pharmacies prescription drugs or mexican rx online
https://maps.google.lk/url?q=https://mexicanpharmacy.shop mexico drug stores pharmacies
mexican online pharmacies prescription drugs mexican rx online and pharmacies in mexico that ship to usa buying prescription drugs in mexico
top online pharmacy india: Online medicine order – online shopping pharmacy india
mexican mail order pharmacies: cheapest mexico drugs – buying prescription drugs in mexico
Well I truly enjoyed reading it. This tip provided by you is very practical for proper planning.
safe online pharmacies in canada northwest canadian pharmacy or reliable canadian pharmacy
https://clients1.google.dm/url?sa=t&url=https://canadianpharmacy24.store canadian pharmacy oxycodone
safe canadian pharmacies canadapharmacyonline com and canadianpharmacyworld canadian pharmacy in canada
best rated canadian pharmacy: Licensed Canadian Pharmacy – my canadian pharmacy reviews
buy prescription drugs from india indian pharmacy delivery top 10 pharmacies in india
https://canadianpharmacy24.store/# canadian pharmacy 24h com
pharmacy website india: Generic Medicine India to USA – buy medicines online in india
pharmacy com canada: Licensed Canadian Pharmacy – legit canadian pharmacy
india online pharmacy cheapest online pharmacy india or п»їlegitimate online pharmacies india
https://clients1.google.ac/url?q=https://indianpharmacy.icu indian pharmacy paypal
indian pharmacies safe indian pharmacy and cheapest online pharmacy india cheapest online pharmacy india
buy prescription drugs from india indian pharmacy delivery indian pharmacies safe
mexican rx online: Online Pharmacies in Mexico – buying prescription drugs in mexico
onlinepharmaciescanada com canada pharmacy online or thecanadianpharmacy
https://cse.google.dj/url?q=https://canadianpharmacy24.store canada drug pharmacy
canada pharmacy 24h canadian pharmacy 24h com safe and trusted canadian pharmacy rate canadian pharmacies
https://canadianpharmacy24.store/# reliable canadian pharmacy
pharmacy website india: Generic Medicine India to USA – world pharmacy india
As I web-site possessor I believe the content material here is rattling excellent , appreciate it for your hard work. You should keep it up forever! Good Luck.
medication from mexico pharmacy cheapest mexico drugs mexican pharmaceuticals online
mexico pharmacies prescription drugs mexican pharmaceuticals online or reputable mexican pharmacies online
https://www.google.co.id/url?sa=t&url=https://mexicanpharmacy.shop mexican mail order pharmacies
buying prescription drugs in mexico mexican pharmacy and mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa
buying prescription drugs in mexico: Mexican Pharmacy Online – mexican rx online
canadian king pharmacy Prescription Drugs from Canada reputable canadian online pharmacy
https://zithromaxall.shop/# zithromax capsules australia
buy amoxicillin 500mg uk: amoxicillin medicine over the counter – generic amoxil 500 mg
generic zithromax india buy zithromax 500mg online zithromax drug
http://zithromaxall.com/# zithromax 500 mg for sale
cost of prednisone: prednisone cost us – cost of prednisone 10mg tablets
http://amoxilall.com/# amoxicillin online without prescription
prednisone ordering online prednisone brand name us how can i get prednisone
1. Вибір натяжних стель: як вибрати ідеальний варіант?
2. Модні тренди натяжних стель на поточний сезон
3. Які переваги мають натяжні стелі порівняно зі звичайними?
4. Як підібрати кольори для натяжної стелі у квартирі?
5. Секрети догляду за натяжними стелями: що потрібно знати?
6. Як зробити вибір між матовими та глянцевими натяжними стелями?
7. Натяжні стелі в інтер’єрі: як вони змінюють приміщення?
8. Натяжні стелі для ванної кімнати: плюси та мінуси
9. Як підняти стеля візуально за допомогою натяжної конструкції?
10. Як вибрати правильний дизайн натяжної стелі для кухні?
11. Інноваційні технології виробництва натяжних стель: що варто знати?
12. Чому натяжні стелі вибирають для офісних приміщень?
13. Натяжні стелі з фотопринтом: які переваги цієї технології?
14. Дизайнерські рішення для натяжних стель: ідеї для втілення
15. Хімічні реагенти в складі натяжних стель: безпека та якість
16. Як вибрати натяжну стелю для дитячої кімнати: поради батькам
17. Які можливості для дизайну приміщень відкривають натяжні стелі?
18. Як впливає вибір матеріалу на якість натяжної стелі?
19. Інструкція з монтажу натяжних стель власноруч: крок за кроком
20. Натяжні стелі як елемент екстер’єру будівлі: переваги та недоліки
натяжні стелі львів відгуки http://www.natjazhnistelifvgtg.lviv.ua .
http://prednisoneall.com/# prednisone nz
clomid tablet: can you buy generic clomid – can i get clomid pill
generic zithromax india zithromax 500 mg lowest price drugstore online zithromax 250 mg tablet price
https://zithromaxall.shop/# how to buy zithromax online
amoxicillin cost australia amoxicillin 500 mg or amoxicillin 500 mg cost
http://loginza.ru/api/widget/?token_url=http://amoxilall.shop amoxicillin script
canadian pharmacy amoxicillin order amoxicillin online no prescription and amoxicillin without rx amoxicillin online without prescription
https://amoxilall.shop/# amoxicillin 1000 mg capsule
buy zithromax online cheap can you buy zithromax over the counter how to get zithromax over the counter
http://amoxilall.com/# buy amoxicillin online cheap
average cost of generic zithromax zithromax for sale usa or how to get zithromax over the counter
https://www.google.com.vn/url?q=https://zithromaxall.shop zithromax 1000 mg pills
buy cheap zithromax online zithromax capsules 250mg and zithromax buy online buy zithromax online fast shipping
zithromax online: zithromax 250 price – zithromax 250 mg
can you get clomid for sale can you buy clomid without a prescription cost of cheap clomid no prescription
https://zithromaxall.com/# can i buy zithromax over the counter in canada
https://zithromaxall.shop/# zithromax online paypal
where can i buy amoxicillin online amoxicillin medicine over the counter or where can i buy amoxicillin over the counter
https://cse.google.lu/url?sa=t&url=https://amoxilall.shop where can i buy amoxocillin
buy amoxicillin 250mg amoxicillin 500 coupon and amoxicillin 500 mg price how much is amoxicillin prescription
where can i buy cheap clomid price order cheap clomid without prescription can you buy clomid now
https://zithromaxall.shop/# zithromax over the counter canada
generic prednisone tablets: can you buy prednisone over the counter uk – prednisone 60 mg daily
демонтаж москва
https://demontagmoskva.ru/
abilify discount cards
https://zithromaxall.shop/# zithromax 500 mg for sale
cost of amoxicillin 30 capsules canadian pharmacy amoxicillin can i buy amoxicillin over the counter in australia
http://amoxilall.com/# amoxicillin 500 mg online
cost clomid no prescription where buy generic clomid price or where buy clomid price
https://maps.google.ws/url?sa=t&rct=j&url=https://clomidall.shop can you get clomid tablets
cost clomid price how to get clomid without a prescription and buying generic clomid without insurance where buy generic clomid pill
prednisone without prescription.net: prednisone 475 – prednisone without prescription medication
can you get cheap clomid buying cheap clomid without insurance cost cheap clomid pills
https://zithromaxall.shop/# zithromax capsules 250mg
actos leaflet
generic amoxicillin online amoxicillin script or how much is amoxicillin prescription
http://wap.didrov.ru/go.php?url=https://amoxilall.shop amoxicillin 500 mg
amoxicillin 500 coupon buy amoxicillin canada and buy amoxil amoxicillin 200 mg tablet
https://zithromaxall.com/# zithromax 500 mg lowest price drugstore online
zithromax 500 mg for sale zithromax tablets for sale buy zithromax without presc
order viagra: best price on viagra – over the counter sildenafil
п»їcialis generic cialis without a doctor prescription buy cialis pill
Kamagra 100mg price: Kamagra gel – Kamagra 100mg price
Cheap generic Viagra online: generic sildenafil – buy Viagra online
https://kamagraiq.shop/# Kamagra 100mg price
Kamagra 100mg price Kamagra Oral Jelly Price Kamagra 100mg
Buy Cialis online: Buy Cialis online – Buy Cialis online
acarbose classe
Generic Cialis without a doctor prescription: cheapest cialis – Buy Tadalafil 10mg
sustain 8 semaglutide
Generic Tadalafil 20mg price cialis without a doctor prescription Tadalafil Tablet
Buy Tadalafil 10mg: cialis without a doctor prescription – cialis generic
buy kamagra online usa: Kamagra Iq – п»їkamagra
https://sildenafiliq.xyz/# Sildenafil 100mg price
buy Kamagra Sildenafil Oral Jelly п»їkamagra
Tadalafil price: Tadalafil price – Generic Tadalafil 20mg price
Kamagra 100mg price: Kamagra gel – cheap kamagra
buy Viagra over the counter sildenafil iq Viagra Tablet price
Kamagra Oral Jelly: Kamagra Oral Jelly Price – sildenafil oral jelly 100mg kamagra
http://sildenafiliq.xyz/# п»їBuy generic 100mg Viagra online
п»їcialis generic Buy Cialis online Tadalafil price
Sildenafil Citrate Tablets 100mg buy Viagra online or Cheap generic Viagra
https://www.google.is/url?q=https://sildenafiliq.com Sildenafil Citrate Tablets 100mg
cheapest viagra Cheap generic Viagra and cheap viagra Generic Viagra online
cialis for sale: Generic Tadalafil 20mg price – Generic Cialis without a doctor prescription
https://kamagraiq.shop/# buy kamagra online usa
buy kamagra online usa: Kamagra gel – Kamagra 100mg price
buy viagra here: generic ed pills – sildenafil online
http://tadalafiliq.com/# cheapest cialis
Kamagra 100mg price kamagra best price sildenafil oral jelly 100mg kamagra
Cialis 20mg price in USA: Generic Tadalafil 20mg price – Cialis 20mg price
cheapest viagra: generic ed pills – viagra without prescription
https://kamagraiq.com/# Kamagra 100mg
Cialis without a doctor prescription tadalafil iq Tadalafil price
Kamagra 100mg price: Kamagra gel – Kamagra 100mg
http://tadalafiliq.com/# Tadalafil price
Приветики!
Диплом Актера Купить
Мы изготавливаем дипломы ВУЗов, техникумов, колледжей, аттестаты о среднем образовании на высококачественных типографских бланках, а так же на оригинальных бланках типографии ГОЗНАК.https://saksx-diploms-srednee24.com/ Диплом магистра даёт возможность параллельно с основной работой вести научно исследовательскую деятельность.но юридически обосновать повышение квалификационного диплома Актера Купить может лишь удостоверение повышение квалификации либо свидетельствования, которые ему идентичны.
Sildenafil Citrate Tablets 100mg Viagra online price or order viagra
https://images.google.ng/url?q=https://sildenafiliq.com Viagra Tablet price
Viagra online price buy viagra here and sildenafil over the counter buy Viagra online
Generic Viagra online: best price on viagra – Viagra online price
Cialis without a doctor prescription cialis best price Cheap Cialis
http://sildenafiliq.xyz/# cheap viagra
http://tadalafiliq.com/# Tadalafil price
buy cialis pill Cialis 20mg price in USA or buy cialis pill
https://www.google.im/url?q=https://tadalafiliq.com Cialis over the counter
cialis for sale Cialis without a doctor prescription and Cialis 20mg price in USA Tadalafil Tablet
generic sildenafil: buy viagra online – buy Viagra over the counter
Cialis over the counter: Generic Cialis without a doctor prescription – Generic Tadalafil 20mg price
sildenafil online sildenafil iq Buy Viagra online cheap
order viagra: generic ed pills – Viagra without a doctor prescription Canada
https://sildenafiliq.com/# Cheap generic Viagra
Viagra online price: buy viagra online – Viagra online price
https://canadianpharmgrx.com/# canadian pharmacy prices
reputable mexican pharmacies online Pills from Mexican Pharmacy mexican pharmacy
mexico pharmacies prescription drugs: online pharmacy in Mexico – mexican drugstore online
msds of repaglinide
https://canadianpharmgrx.com/# canadian drugs online
pharmacies in canada that ship to the us: Certified Canadian pharmacies – canada drugs
canada drugs online Canada pharmacy canadian pharmacy tampa
my canadian pharmacy canadian pharmacies comparison or safe canadian pharmacy
https://maps.google.pn/url?sa=t&url=https://canadianpharmgrx.com the canadian pharmacy
online canadian pharmacy reviews canadian family pharmacy and escrow pharmacy canada onlinecanadianpharmacy 24
https://canadianpharmgrx.com/# best online canadian pharmacy
reputable indian online pharmacy indian pharmacy delivery best online pharmacy india
is remeron an maoi
https://canadianpharmgrx.xyz/# best online canadian pharmacy
Do you have a spam problem on this site; I also am a blogger, and I was wanting to know your situation; we have created some nice practices and we are looking to trade techniques with others, be sure to shoot me an email if interested.
Привет всем!
Бывали ли у вас случаи, когда приходилось писать дипломную работу в крайне сжатые сроки? Это действительно требует большой ответственности и напряженного труда, но важно не унывать и продолжать активно участвовать в учебном процессе, как я и делаю.
Для тех, кто умеет эффективно находить и использовать информацию в интернете, это может существенно облегчить процесс согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или организацию встреч с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на https://rudik-diploms365.com, это проверено!
https://gruppa365-diploms-srednee.com/
купить диплом Вуза
купить диплом университета
купить диплом колледжа
где купить диплом
купить диплом о среднем специальном
Желаю любому положительных отметок!
http://canadianpharmgrx.xyz/# canadian pharmacy meds
medication canadian pharmacy International Pharmacy delivery canadian pharmacy ltd
best india pharmacy: Healthcare and medicines from India – india pharmacy
https://indianpharmgrx.shop/# buy medicines online in india
canadian pharmacy 365: My Canadian pharmacy – canadian pharmacies comparison
top online pharmacy india india online pharmacy world pharmacy india
northern pharmacy canada canada pharmacy world or canadian pharmacy 1 internet online drugstore
https://images.google.tn/url?q=https://canadianpharmgrx.com canadian online drugs
canada pharmacy canadian king pharmacy and canadian pharmacy canadian pharmacy service
mexico drug stores pharmacies mexico drug stores pharmacies or buying prescription drugs in mexico
http://www.rpklublin.pl/skins/rpk/redirect.php?url=http://mexicanpharmgrx.com buying prescription drugs in mexico
medication from mexico pharmacy best online pharmacies in mexico and buying prescription drugs in mexico mexican mail order pharmacies
https://indianpharmgrx.shop/# top 10 online pharmacy in india
robaxin 500mg street value
otc protonix
online canadian pharmacy International Pharmacy delivery canada pharmacy world
https://mexicanpharmgrx.com/# buying from online mexican pharmacy
best india pharmacy buy medicines online in india or indian pharmacy
http://www.google.com.pg/url?sa=i&rct=j&q=&esrc=s&source=images&cd=&cad=rja&uact=8&docid=zuid2ho-0hgt1m&tbnid=kc9iiu4fp5ainm:&ved=0cacqjrw&url=http://indianpharmgrx.com&ei=nvavvktgends8awt04d4cq&bvm=b best india pharmacy
world pharmacy india world pharmacy india and indian pharmacy paypal Online medicine home delivery
best online pharmacies in mexico mexican pharmacy buying prescription drugs in mexico online
п»їlegitimate online pharmacies india: indian pharmacy delivery – cheapest online pharmacy india
http://indianpharmgrx.com/# best india pharmacy
buying drugs from canada Certified Canadian pharmacies best canadian online pharmacy reviews
indian pharmacy: Healthcare and medicines from India – india online pharmacy
canadian pharmacy antibiotics canada pharmacy 24h or cheap canadian pharmacy
http://www.google.com.uy/url?q=http://canadianpharmgrx.com online canadian pharmacy
canada drugs online review canada cloud pharmacy and canada pharmacy online canadian drug stores
https://mexicanpharmgrx.shop/# best online pharmacies in mexico
https://canadianpharmgrx.xyz/# reliable canadian pharmacy
indianpharmacy com Generic Medicine India to USA buy prescription drugs from india
northwest pharmacy canada canadian discount pharmacy or canadian drug pharmacy
https://www.ahewar.org/links/dform.asp?url=https://canadianpharmgrx.xyz onlinepharmaciescanada com
canadian pharmacy mall ordering drugs from canada and reputable canadian online pharmacy best canadian pharmacy to buy from
http://mexicanpharmgrx.com/# mexico pharmacies prescription drugs
My spouse and I stumbled over here coming from a different web page and thought I should check things out. I like what I see so i am just following you. Look forward to exploring your web page yet again.
canada drug pharmacy My Canadian pharmacy canadian pharmacy drugs online
http://mexicanpharmgrx.shop/# mexican pharmacy
best india pharmacy: online pharmacy india – india pharmacy
Wow! After all I got a website from where I be able to really obtain useful facts regarding my study and knowledge.
indian pharmacy paypal: indian pharmacy – cheapest online pharmacy india
http://mexicanpharmgrx.shop/# mexican mail order pharmacies
canadian pharmacy online legal to buy prescription drugs from canada or legal to buy prescription drugs from canada
http://www.dmxmc.de/url?q=https://canadianpharmgrx.com canada pharmacy online
canada rx pharmacy world canada cloud pharmacy and canadian pharmacy uk delivery ed drugs online from canada
natural alternatives to tamoxifen: nolvadex estrogen blocker – tamoxifen estrogen
how to order doxycycline doxylin doxy 200
diflucan generic: where to buy diflucan otc – buy diflucan over the counter
dcis tamoxifen: tamoxifen endometriosis – tamoxifen citrate pct
where to get doxycycline where can i get doxycycline where to get doxycycline
Привет всем!
Бывали ли у вас случаи, когда приходилось писать дипломную работу в крайне сжатые сроки? Это действительно требует большой ответственности и напряженного труда, но важно не унывать и продолжать активно участвовать в учебном процессе, как я и делаю.
Для тех, кто умеет эффективно находить и использовать информацию в интернете, это может существенно облегчить процесс согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или организацию встреч с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на , это проверено!
https://landik-diploms-srednee24.com/
купить диплом цена
купить диплом института
купить аттестат школы
где купить диплом
купить диплом о среднем образовании
Желаю любому пятерошных) оценок!
buy diflucan medicarions: can i buy diflucan without a prescription – where can i buy diflucan without a prescription
https://misoprostol.top/# cytotec pills buy online
cipro buy cipro online without prescription buy ciprofloxacin over the counter
buy ciprofloxacin over the counter: cipro 500mg best prices – ciprofloxacin
buy cipro purchase cipro or buy generic ciprofloxacin
http://alpha.astroempires.com/redirect.aspx?https://ciprofloxacin.guru/ cipro
cipro antibiotics cipro and ciprofloxacin 500 mg tablet price ciprofloxacin order online
how to order doxycycline: doxy – doxycycline 100mg
tamoxifen for men: tamoxifen menopause – nolvadex vs clomid
tamoxifen for men nolvadex during cycle tamoxifen citrate
cytotec pills buy online cytotec online or purchase cytotec
http://start.midnitemusic.ch/index.php?url=http://misoprostol.top Misoprostol 200 mg buy online
buy cytotec online fast delivery Cytotec 200mcg price and buy cytotec cytotec abortion pill
п»їcytotec pills online buy cytotec pills online cheap buy cytotec over the counter
synthroid 88 mcg cost
buy cipro online: ciprofloxacin order online – buy cipro online without prescription
doxycycline 100mg doxycycline hydrochloride 100mg or online doxycycline
https://cse.google.com.pg/url?sa=t&url=https://doxycyclinest.pro vibramycin 100 mg
where to get doxycycline doxy 200 and buy doxycycline online 270 tabs doxycycline generic
canadian pharmacy ed medications
https://misoprostol.top/# buy cytotec online fast delivery
lisinopril 50 mg
buy cytotec: buy cytotec pills – Misoprostol 200 mg buy online
diflucan pill diflucan tablets buy online buy diflucan yeast infection
Cytotec 200mcg price: п»їcytotec pills online – buy cytotec
1. Идеи для дизайна интерьера
2. Топ-20 трендов в дизайне на 2021 год
3. Как выбрать идеальный цветовой акцент в дизайне
4. Секреты успешного дизайн-проекта
5. Инновационные подходы к дизайну: отражение современности
6. Шаг за шагом: создание уютного дизайна спальни
7. Дизайнерские решения для увеличения пространства в маленькой квартире
8. Природный дизайн
9. Баланс цветов и форм: основы хорошего дизайна
10. Дизайн-студия: секреты успешного бизнеса в сфере дизайна
11. Дизайн в XXI веке
12. Дизайн кухни
13. Дизайн мебели
14. Мастер-класс по созданию стильного дизайна гостиной
15. Минимализм
16. Дизайн сада
17. Декорирование с текстилем
18. Принципы цветового баланса в дизайне: как создать гармоничное пространство
19. Топ-10 книг по дизайну интерьера, которые стоит прочитать
20. Дизайн подростковой комнаты
студия интерьеров https://studiya-dizajna-intererov.ru/ .
buy generic ciprofloxacin: ciprofloxacin order online – cipro pharmacy
diflucan 150 mg otc diflucan cream prescription diflucan brand name
ciprofloxacin order online: buy cipro cheap – ciprofloxacin mail online
is nolvadex legal tamoxifen and grapefruit or nolvadex 10mg
http://ggeek.ru/bitrix/redirect.php?event1=&event2=&event3=&goto=https://nolvadex.icu where to get nolvadex
where to buy nolvadex buy nolvadex online and tamoxifen side effects forum tamoxifen generic
synthroid 0.025
diflucan 150 tab: diflucan tabs – diflucan 6
buy cipro online canada purchase cipro or cipro ciprofloxacin
https://maps.google.bj/url?sa=t&url=https://ciprofloxacin.guru ciprofloxacin over the counter
ciprofloxacin generic buy cipro online canada and cipro pharmacy cipro for sale
https://misoprostol.top/# cytotec buy online usa
tamoxifen generic does tamoxifen cause joint pain tamoxifen chemo
tamoxifen side effects forum: tamoxifen and osteoporosis – tamoxifen medication
azithromycin otc usa
doxycycline 50 mg doxycycline hyclate where to get doxycycline
can i buy prednisone online in uk
price of azithromycin tablets
<a href="[Link deleted]pharmacy online
<a href="[Link deleted]20 mg over the counter
<a href="[Link deleted]canada cost
<a href="[Link deleted]2018
<a href="[Link deleted]online pharmacy free shipping
<a href="[Link deleted]indian online pharmacy
<a href="[Link deleted]launch
<a href="[Link deleted]tabs
<a href="[Link deleted]online thai pharmacy
<a href="[Link deleted]prednisone online
<a href="[Link deleted]can i buy azithromycin pills
<a href="[Link deleted]prednisone
<a href="[Link deleted]pharmacy for prescriptions without insurance
<a href="[Link deleted]azithromycin over the counter
<a href="[Link deleted]metformin 1000 mg
<a href="[Link deleted]75 mcg tablet price
<a href="[Link deleted]without prescription
<a href="[Link deleted]happy family store pharmacy
На сегодняшний день, когда диплом – это начало отличной карьеры в любом направлении, многие пытаются найти максимально быстрый путь получения образования. Наличие официального документа об образовании сложно переоценить. Ведь именно он открывает двери перед людьми, стремящимися вступить в сообщество профессиональных специалистов или продолжить обучение в ВУЗе.
Мы предлагаем оперативно получить этот важный документ. Вы имеете возможность купить диплом, и это является выгодным решением для человека, который не смог завершить образование или утратил документ. Все дипломы выпускаются аккуратно, с особым вниманием к мельчайшим деталям, чтобы в итоге получился документ, 100% соответствующий оригиналу.
Превосходство этого решения состоит не только в том, что вы сможете быстро получить свой диплом. Весь процесс организовывается просто и легко, с профессиональной поддержкой. Начав от выбора подходящего образца до грамотного заполнения персональной информации и доставки в любое место страны — все под полным контролем качественных мастеров.
Для всех, кто хочет найти максимально быстрый способ получения необходимого документа, наша компания может предложить отличное решение. Приобрести диплом – это значит избежать долгого процесса обучения и сразу переходить к личным целям, будь то поступление в ВУЗ или старт трудовой карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
В нашем мире, где диплом является началом удачной карьеры в любой отрасли, многие ищут максимально быстрый и простой путь получения качественного образования. Наличие документа об образовании переоценить просто невозможно. Ведь диплом открывает двери перед людьми, желающими начать трудовую деятельность или продолжить обучение в любом институте.
Мы предлагаем очень быстро получить этот важный документ. Вы имеете возможность купить диплом нового или старого образца, и это будет отличным решением для всех, кто не смог завершить обучение, утратил документ или хочет исправить свои оценки. дипломы производятся с особой тщательностью, вниманием ко всем нюансам, чтобы на выходе получился полностью оригинальный документ.
Преимущества этого подхода заключаются не только в том, что вы максимально быстро получите свой диплом. Процесс организован просто и легко, с нашей поддержкой. От выбора необходимого образца до консультации по заполнению персональных данных и доставки по России — все под абсолютным контролем качественных мастеров.
В итоге, для тех, кто пытается найти быстрый и простой способ получения необходимого документа, наша компания готова предложить выгодное решение. Заказать диплом – значит избежать продолжительного обучения и сразу переходить к своим целям: к поступлению в ВУЗ или к началу трудовой карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
На сегодняшний день, когда диплом становится началом успешной карьеры в любой отрасли, многие стараются найти максимально быстрый и простой путь получения образования. Факт наличия официального документа переоценить попросту невозможно. Ведь диплом открывает дверь перед любым человеком, желающим начать трудовую деятельность или учиться в любом ВУЗе.
В данном контексте наша компания предлагает быстро получить этот важный документ. Вы можете приобрести диплом, и это является выгодным решением для человека, который не смог закончить обучение или утратил документ. Все дипломы выпускаются с особой аккуратностью, вниманием ко всем деталям. В результате вы получите документ, максимально соответствующий оригиналу.
Превосходство подобного решения заключается не только в том, что можно быстро получить диплом. Весь процесс организовывается удобно, с нашей поддержкой. От выбора нужного образца до консультаций по заполнению персональной информации и доставки по России — все под полным контролем квалифицированных специалистов.
Таким образом, для тех, кто ищет максимально быстрый способ получить требуемый документ, наша компания готова предложить выгодное решение. Приобрести диплом – это значит избежать длительного процесса обучения и не теряя времени перейти к достижению личных целей: к поступлению в ВУЗ или к началу трудовой карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
В нашем обществе, где диплом – это начало удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения качественного образования. Необходимость наличия официального документа переоценить просто невозможно. Ведь именно диплом открывает двери перед всеми, кто собирается вступить в профессиональное сообщество или продолжить обучение в университете.
Мы предлагаем оперативно получить этот важный документ. Вы можете приобрести диплом, что будет удачным решением для всех, кто не смог закончить образование, потерял документ или желает исправить плохие оценки. Любой диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям. На выходе вы получите документ, 100% соответствующий оригиналу.
Превосходство подобного решения заключается не только в том, что вы сможете оперативно получить свой диплом. Весь процесс организован комфортно, с профессиональной поддержкой. От выбора подходящего образца до грамотного заполнения личной информации и доставки в любой регион России — все находится под полным контролем опытных мастеров.
Для всех, кто ищет быстрый и простой способ получить необходимый документ, наша компания предлагает выгодное решение. Заказать диплом – значит избежать продолжительного процесса обучения и сразу перейти к достижению личных целей, будь то поступление в университет или начало удачной карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
Сегодня, когда диплом – это начало удачной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Наличие официального документа об образовании трудно переоценить. Ведь диплом открывает двери перед людьми, желающими вступить в профессиональное сообщество или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает оперативно получить любой необходимый документ. Вы имеете возможность приобрести диплом, и это будет удачным решением для всех, кто не смог завершить обучение, потерял документ или хочет исправить свои оценки. Все дипломы производятся аккуратно, с особым вниманием к мельчайшим элементам. В результате вы сможете получить продукт, полностью соответствующий оригиналу.
Плюсы такого решения состоят не только в том, что можно оперативно получить свой диплом. Процесс организован комфортно, с профессиональной поддержкой. От выбора необходимого образца до консультаций по заполнению личной информации и доставки в любое место страны — все под абсолютным контролем опытных мастеров.
Всем, кто ищет оперативный способ получения требуемого документа, наша компания готова предложить отличное решение. Заказать диплом – значит избежать длительного процесса обучения и не теряя времени перейти к достижению своих целей, будь то поступление в ВУЗ или старт карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
<a href=[Link deleted]
В современном мире, где диплом становится началом успешной карьеры в любом направлении, многие ищут максимально простой путь получения качественного образования. Факт наличия документа об образовании трудно переоценить. Ведь именно он открывает дверь перед каждым человеком, желающим вступить в сообщество профессионалов или продолжить обучение в высшем учебном заведении.
В данном контексте мы предлагаем быстро получить этот важный документ. Вы можете купить диплом, и это является удачным решением для всех, кто не смог закончить обучение, утратил документ или хочет исправить свои оценки. диплом изготавливается с особой аккуратностью, вниманием ко всем деталям. В результате вы получите 100% оригинальный документ.
Преимущество данного подхода состоит не только в том, что вы максимально быстро получите диплом. Процесс организован удобно, с нашей поддержкой. От выбора необходимого образца документа до консультации по заполнению персональной информации и доставки по России — все находится под абсолютным контролем опытных специалистов.
Для всех, кто хочет найти оперативный способ получить требуемый документ, наша компания предлагает отличное решение. Заказать диплом – значит избежать продолжительного процесса обучения и сразу перейти к достижению собственных целей, будь то поступление в университет или начало карьеры.
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
[Link deleted]
<a href=[Link deleted]watches
Understanding COSC Accreditation and Its Importance in Watchmaking
COSC Certification and its Rigorous Standards
Controle Officiel Suisse des Chronometres, or the Controle Officiel Suisse des Chronometres, is the official Swiss testing agency that attests to the precision and accuracy of wristwatches. COSC certification is a mark of quality craftsmanship and trustworthiness in timekeeping. Not all watch brands seek COSC certification, such as Hublot, which instead follows to its proprietary demanding criteria with mechanisms like the UNICO, attaining equivalent precision.
The Art of Precision Chronometry
The core system of a mechanical watch involves the spring, which delivers power as it unwinds. This mechanism, however, can be prone to environmental elements that may impact its precision. COSC-certified mechanisms undergo demanding testing—over 15 days in various conditions (5 positions, three temperatures)—to ensure their resilience and dependability. The tests assess:
Average daily rate precision between -4 and +6 seconds.
Mean variation, maximum variation rates, and impacts of thermal variations.
Why COSC Validation Is Important
For timepiece aficionados and collectors, a COSC-accredited watch isn’t just a item of tech but a demonstration to enduring quality and accuracy. It signifies a timepiece that:
Presents excellent dependability and accuracy.
Ensures assurance of superiority across the complete design of the timepiece.
Is likely to retain its worth more effectively, making it a sound investment.
Popular Chronometer Manufacturers
Several famous brands prioritize COSC accreditation for their timepieces, including Rolex, Omega, Breitling, and Longines, among others. Longines, for instance, presents collections like the Record and Soul, which highlight COSC-accredited movements equipped with advanced substances like silicon balance springs to improve durability and efficiency.
Historic Background and the Evolution of Chronometers
The idea of the timepiece originates back to the requirement for exact timekeeping for navigation at sea, emphasized by John Harrison’s work in the eighteenth cent. Since the formal foundation of COSC in 1973, the validation has become a benchmark for judging the precision of luxury watches, maintaining a legacy of excellence in horology.
Conclusion
Owning a COSC-certified timepiece is more than an aesthetic choice; it’s a commitment to quality and accuracy. For those valuing accuracy above all, the COSC accreditation provides tranquility of mind, guaranteeing that each accredited watch will function reliably under various conditions. Whether for individual contentment or as an investment, COSC-validated timepieces distinguish themselves in the world of horology, maintaining on a tradition of meticulous chronometry.
<a href=[Link deleted]
Son Dönemsel En Popüler Bahis Sitesi: Casibom
Kumarhane oyunlarını sevenlerin artık duymuş olduğu Casibom, en son dönemde adından çoğunlukla söz ettiren bir iddia ve casino sitesi haline geldi. Ülkemizin en mükemmel casino sitelerinden biri olarak tanınan Casibom'un haftalık göre değişen açılış adresi, alanında oldukça taze olmasına rağmen itimat edilir ve kazandıran bir platform olarak tanınıyor.
Casibom, yakın rekabeti olanları geride kalarak köklü bahis sitelerinin geride bırakmayı başarılı oluyor. Bu sektörde eski olmak önemlidir olsa da, katılımcılarla iletişim kurmak ve onlara erişmek da benzer miktar önemlidir. Bu aşamada, Casibom'un 7/24 hizmet veren gerçek zamanlı destek ekibi ile kolayca iletişime temas kurulabilir olması önemli bir avantaj sunuyor.
Süratle artan oyuncu kitlesi ile dikkat çeken Casibom'un arka planında başarılı faktörleri arasında, sadece ve yalnızca kumarhane ve gerçek zamanlı casino oyunlarıyla sınırlı olmayan kapsamlı bir hizmetler yelpazesi bulunuyor. Sporcular bahislerinde sunduğu geniş seçenekler ve yüksek oranlar, oyuncuları cezbetmeyi başarıyor.
Ayrıca, hem atletizm bahisleri hem de bahis oyunları oyuncularına yönlendirilen sunulan yüksek yüzdeli avantajlı bonuslar da dikkat çekiyor. Bu nedenle, Casibom kısa sürede alanında iyi bir pazarlama başarısı elde ediyor ve önemli bir oyuncu kitlesi kazanıyor.
Casibom'un kar getiren bonusları ve tanınırlığı ile birlikte, web sitesine abonelik nasıl sağlanır sorusuna da bahsetmek gereklidir. Casibom'a mobil cihazlarınızdan, bilgisayarlarınızdan veya tabletlerinizden tarayıcı üzerinden kolayca erişilebilir. Ayrıca, platformun mobil uyumlu olması da büyük bir artı sağlıyor, çünkü artık hemen hemen herkesin bir akıllı telefonu var ve bu cihazlar üzerinden kolayca giriş sağlanabiliyor.
Taşınabilir cep telefonlarınızla bile yolda canlı bahisler alabilir ve maçları gerçek zamanlı olarak izleyebilirsiniz. Ayrıca, Casibom'un mobil uyumlu olması, memleketimizde kumarhane ve casino gibi yerlerin yasal olarak kapatılmasıyla birlikte bu tür platformlara erişimin önemli bir yolunu oluşturuyor.
Casibom'un güvenilir bir casino web sitesi olması da önemlidir bir avantaj getiriyor. Ruhsatlı bir platform olan Casibom, duraksız bir şekilde eğlence ve kazanç elde etme imkanı sağlar.
Casibom'a abone olmak da oldukça basittir. Herhangi bir belge gereksinimi olmadan ve ücret ödemeden web sitesine kolayca abone olabilirsiniz. Ayrıca, site üzerinde para yatırma ve çekme işlemleri için de çok sayıda farklı yöntem mevcuttur ve herhangi bir kesim ücreti talep edilmemektedir.
Ancak, Casibom'un güncel giriş adresini izlemek de elzemdir. Çünkü canlı şans ve kumarhane siteleri popüler olduğu için hileli siteler ve dolandırıcılar da ortaya çıkmaktadır. Bu nedenle, Casibom'un sosyal medya hesaplarını ve güncel giriş adresini düzenli olarak kontrol etmek elzemdir.
Sonuç olarak, Casibom hem güvenilir hem de kazandıran bir kumarhane platformu olarak ilgi çekiyor. yüksek bonusları, geniş oyun seçenekleri ve kullanıcı dostu mobil uygulaması ile Casibom, casino sevenler için mükemmel bir platform sunuyor.
LhaneGax
Здравствуйте!
Для диплома интернет стал источником полезных ресурсов, облегчивших задачу.
Предлагаем всем желающим приобрести диплом университета России по выгодной цене с доставкой “под ключ”.
Желаю каждому не двоешных) оценок!
купить диплом в якутске
купить диплом в мытищах
купить диплом в челябинске
купить диплом в белорецке
купить диплом в ростове-на-дону
<a href=[Link deleted]купить диплом о среднем образование
<a href=[Link deleted]диплом в благовещенске
<a href=[Link deleted]бланк диплома
<a href=[Link deleted]диплом в саратове
<a href=[Link deleted]диплом в балашове
LhaneGax
Привет всем!
Продолжаю трудиться над дипломом, несмотря на все трудности, и благодарен сети за предоставленные ресурсы.
Мы предлагаем купить диплом Гознак со скидкой, гарантией и доставкой в любой город РФ.
Желаю каждому честных оценок!
купить диплом агронома
купить диплом хореографа
купить диплом в новотроицке
купить морской диплом
купить диплом в братске
<a href=[Link deleted]диплом в рязани
<a href=[Link deleted]диплом в салавате
<a href=[Link deleted]диплом о высшем образовании
<a href=[Link deleted]диплом в сочи
<a href=[Link deleted]диплом в липецке
<a href="[Link deleted]pharmacy world coupon
<a href="[Link deleted]synthroid 75 mcg
<a href="[Link deleted]valtrex in mexico
Understanding COSC Certification and Its Importance in Watchmaking
COSC Accreditation and its Demanding Criteria
COSC, or the Official Swiss Chronometer Testing Agency, is the official Switzerland testing agency that attests to the accuracy and precision of timepieces. COSC validation is a sign of quality craftsmanship and trustworthiness in timekeeping. Not all timepiece brands follow COSC accreditation, such as Hublot, which instead adheres to its own strict standards with movements like the UNICO, reaching equivalent accuracy.
The Science of Precision Timekeeping
The core system of a mechanized watch involves the mainspring, which provides energy as it loosens. This system, however, can be susceptible to external elements that may impact its precision. COSC-accredited mechanisms undergo demanding testing—over 15 days in various conditions (5 positions, three temperatures)—to ensure their durability and reliability. The tests evaluate:
Average daily rate accuracy between -4 and +6 secs.
Mean variation, peak variation levels, and impacts of temperature changes.
Why COSC Validation Is Important
For timepiece enthusiasts and connoisseurs, a COSC-certified watch isn’t just a item of tech but a proof to enduring excellence and accuracy. It symbolizes a timepiece that:
Provides outstanding dependability and precision.
Provides confidence of quality across the whole construction of the timepiece.
Is probable to retain its worth more efficiently, making it a wise choice.
Popular Timepiece Manufacturers
Several famous brands prioritize COSC validation for their watches, including Rolex, Omega, Breitling, and Longines, among others. Longines, for instance, offers collections like the Archive and Spirit, which feature COSC-certified movements equipped with advanced materials like silicon equilibrium springs to improve resilience and performance.
Historical Context and the Development of Timepieces
The concept of the timepiece dates back to the need for exact timekeeping for navigation at sea, emphasized by John Harrison’s work in the eighteenth century. Since the official foundation of COSC in 1973, the accreditation has become a benchmark for judging the accuracy of high-end watches, continuing a legacy of excellence in horology.
Conclusion
Owning a COSC-accredited timepiece is more than an aesthetic choice; it’s a commitment to quality and accuracy. For those valuing accuracy above all, the COSC validation provides tranquility of mind, ensuring that each accredited watch will perform dependably under various conditions. Whether for individual contentment or as an investment decision, COSC-validated watches stand out in the world of horology, bearing on a legacy of meticulous chronometry.
<a href="[Link deleted]60 mg daily
you are truly a just right webmaster. The site loading speed is amazing. It seems that you are doing any unique trick. Moreover, The contents are masterwork. you have done a excellent task on this matter!
<a href=[Link deleted]
<a href="[Link deleted]500 mg tablet
<a href="[Link deleted]zithromax 500mg